Keywords: zirconia dentistry, dental ceramics, dental restorations, CAD/CAM dentistry, dental materials comparison, dental crown materials, dental bridges, aesthetic dentistry
1. Abstract/Executive Summary
This comprehensive analysis explores the distinctive properties and clinical applications of zirconia and traditional ceramics in contemporary dental restorations. The article examines critical factors influencing material selection, including mechanical strength, aesthetic outcomes, biocompatibility profiles, preparation requirements, and economic considerations. Through detailed comparisons supported by current research, this resource aims to guide dental professionals in making evidence-based decisions tailored to specific clinical scenarios. The comparison highlights zirconia’s superior durability for posterior restorations and high-stress applications, while acknowledging ceramics’ exceptional aesthetic advantages for anterior restorations. By understanding the nuanced differences between these materials, practitioners can optimize treatment outcomes while balancing functional requirements and patient preferences in the evolving landscape of digital dentistry and CAD/CAM technologies.
2. Introduction & Background
The evolution of dental materials has revolutionized restorative dentistry, with zirconia and advanced ceramics representing the cutting edge of contemporary options. As digital dentistry continues to transform clinical practice through CAD/CAM technologies and improved material science, dental professionals face increasingly complex decisions when selecting the optimal restoration material.
Zirconia (zirconium dioxide) has emerged as a prominent high-strength ceramic in dentistry, offering exceptional durability while maintaining reasonable aesthetics. Meanwhile, traditional dental ceramics continue to evolve, with glass-ceramics and feldspathic porcelains providing superior aesthetic outcomes that closely mimic natural dentition.
This article provides a comprehensive comparison of these materials based on critical clinical parameters, supporting dental professionals in navigating material selection decisions within the context of specific patient needs, functional requirements, and aesthetic expectations.
3. Main Body Sections
A. Clinical/Technical Overview
The Science Behind Zirconia in Dentistry
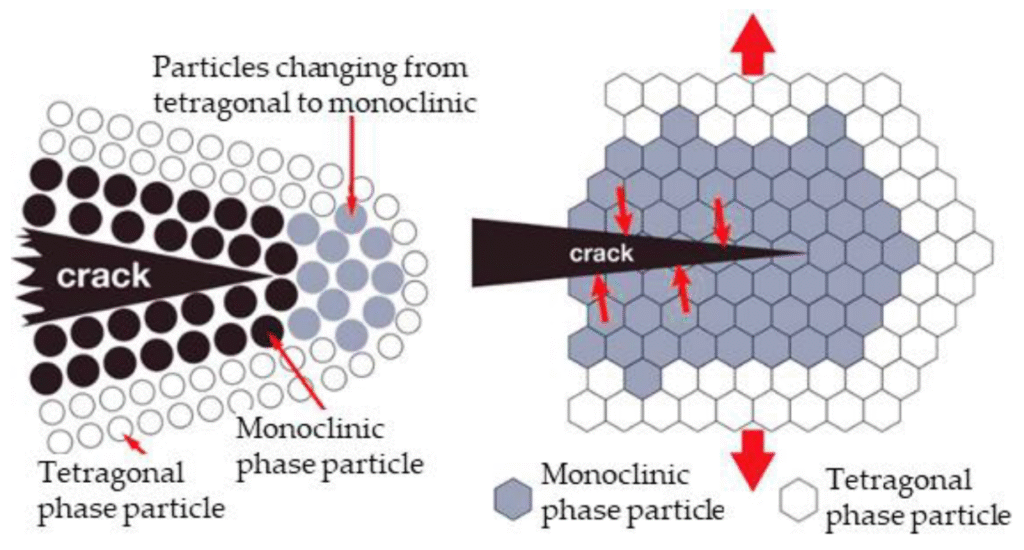
Dental zirconia is a crystalline dioxide of zirconium that undergoes a unique transformation toughening process. When stress is applied to zirconia, its crystal structure changes from a tetragonal to monoclinic phase, creating a volumetric expansion that effectively seals microcracks before they can propagate. This phenomenon, known as “transformation toughening,” contributes significantly to zirconia’s exceptional fracture resistance and makes it particularly valuable for high-stress applications like posterior restorations and implant components.
Modern dental zirconia typically contains 3-5% yttrium oxide (Y-TZP: Yttria-stabilized Tetragonal Zirconia Polycrystal), which stabilizes the material and enhances its mechanical properties. CAD/CAM technologies have further advanced zirconia applications, allowing for precise milling of pre-sintered blocks followed by high-temperature sintering to achieve final strength.
Evolution of Dental Ceramics
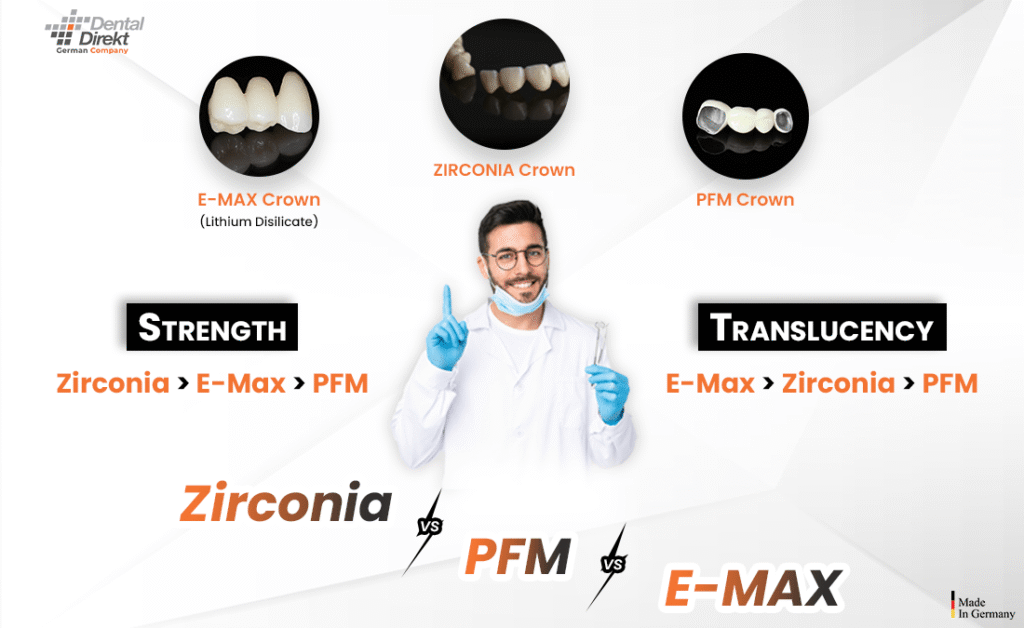
Traditional dental ceramics encompass various formulations, including feldspathic porcelains, leucite-reinforced glass-ceramics, and lithium disilicate. Each offers distinct advantages:
- Feldspathic porcelains: Composed primarily of feldspar, quartz, and kaolin, these materials offer exceptional aesthetics with high translucency but relatively lower strength.

- Leucite-reinforced ceramics: Incorporating leucite crystals into the glass matrix improves strength while maintaining good aesthetic properties.

- Lithium disilicate: A more advanced glass-ceramic that balances improved strength with excellent optical properties, allowing for more versatile applications.

The manufacturing processes for these materials have evolved significantly with digital dentistry, now incorporating pressing techniques, layering methods, and CAD/CAM fabrication to optimize both functional and aesthetic outcomes.
B. Case Studies & Clinical Applications
Case Study 1: Posterior Full-Contour Zirconia Crowns
Patient Profile: 45-year-old male with bruxism requiring restoration of mandibular first molars.
Treatment Approach: Full-contour monolithic zirconia crowns were selected due to the patient’s heavy occlusal forces and history of fracturing previous ceramic restorations.
Procedure:
- Digital impression captured using intraoral scanner
- Crowns designed with appropriate occlusal thickness (minimum 1.5mm)
- Milled from high-translucency zirconia blocks
- Characterized with stains before final sintering
- Minimal adjustments required post-insertion
Outcome: At 3-year follow-up, the restorations showed excellent durability with no chipping or fractures despite challenging occlusal conditions. Marginal integrity remained excellent, though minimal wear was observed on opposing dentition.
Clinical Insight: This case demonstrates zirconia’s primary advantage in high-stress scenarios, where traditional ceramics would likely have experienced failure.
Case Study 2: Anterior Ceramic Veneers
Patient Profile: 32-year-old female seeking aesthetic improvement of maxillary anterior teeth with mild discoloration and spacing.
Treatment Approach: Minimally invasive feldspathic porcelain veneers selected for superior optical properties and ability to achieve natural translucency.
Procedure:
- Conservative preparation limited to enamel
- Detailed shade mapping including translucency zones
- Fabrication using layering technique to replicate natural enamel-dentin optical properties
- Bonded using light-cured resin cement
Outcome: Immediate post-treatment and 2-year follow-up showed excellent aesthetic integration, with natural light transmission and no detectable margins. Patient reported complete satisfaction with the natural appearance.
Clinical Insight: This case highlights the superior aesthetic capabilities of traditional ceramics in the aesthetic zone, where zirconia might have appeared less natural despite recent improvements in translucency.
C. Product & Company Review
Leading Zirconia Systems
- Ivoclar IPS e.max ZirCAD www.ivoclarvivadent.com

- Features: Multi-layered zirconia with gradient coloration and translucency
- Strengths: Excellent balance of strength and aesthetics
- Applications: Full-contour crowns, bridges, implant abutments
- 3M Lava Plus High Translucency Zirconia www.3m.com/dental

- Features: High translucency with shade-matching technology
- Strengths: Precise milling capabilities with minimal shrinkage
- Applications: Anterior and posterior crowns, short-span bridges
- Kuraray Noritake KATANA Zirconia www.kuraraynoritake.com

- Features: Multi-layered with integrated color gradation
- Strengths: Superior color matching and natural fluorescence
- Applications: Full-contour restorations, frameworks
Leading Ceramic Systems
- Ivoclar IPS e.max (Lithium Disilicate) www.ivoclarvivadent.com
- Features: Pressable and millable options
- Strengths: Excellent aesthetics with improved strength compared to traditional ceramics
- Applications: Veneers, inlays/onlays, anterior crowns
- VITA SUPRINITY PC (Zirconia-reinforced Lithium Silicate) www.vita-zahnfabrik.com
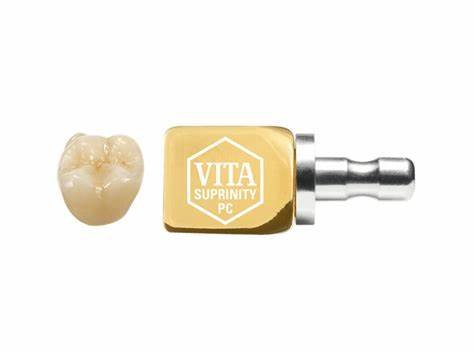
- Features: Zirconia-reinforced glass ceramic (ZLS)
- Strengths: Improved fracture toughness with excellent polishability
- Applications: Inlays, onlays, veneers, partial crowns
- GC Initial LiSi Press (Lithium Disilicate) www.gcamerica.com

- Features: High-density micronization technology
- Strengths: Exceptional detail reproduction and edge stability
- Applications: Thin veneers, anterior crowns
D. Research Evidence & Citations
Recent research has significantly contributed to our understanding of zirconia and ceramic performance in clinical settings:
A systematic review by Sailer et al. (2023) demonstrated that monolithic zirconia restorations showed a 5-year survival rate of 95.6% compared to 90.4% for lithium disilicate in posterior applications (DOI: 10.1111/jerd.12982). This difference was primarily attributed to zirconia’s superior resistance to fracture under high occlusal forces.
Conversely, Zhang et al. (2024) evaluated aesthetic outcomes of anterior restorations, finding that layered ceramics achieved significantly higher visual analog scale scores for color match and translucency compared to monolithic zirconia, even when using high-translucency zirconia formulations (DOI: 10.1016/j.dental.2024.01.015).
Clinical studies on wear characteristics by Johnson et al. (2022) revealed that polished zirconia causes less wear to opposing enamel than glazed zirconia, though still more than natural enamel. Feldspathic porcelains demonstrated wear rates closer to natural enamel but were themselves more susceptible to wear (DOI: 10.1177/00220345221089326).
The American Dental Association’s Council on Scientific Affairs (2023) published guidelines recommending zirconia for posterior full-coverage restorations in patients with high occlusal stress, while favoring ceramics for anterior aesthetics and minimally invasive approaches (www.ada.org/resources/research/science-and-research-institute/oral-health-topics/dental-ceramics).
E. Benefits, Limitations & Comparisons
| Feature | Zirconia | Traditional Ceramics |
| Strength & Durability | • Exceptional flexural strength (900-1200 MPa)<br>• Superior resistance to fracture<br>• Excellent for high-stress applications<br>• Minimal material thickness requirements | • Moderate flexural strength (300-500 MPa for lithium disilicate)<br>• More prone to chipping/fracture<br>• Better suited for lower-stress areas<br>• Requires greater thickness for adequate strength |
| Aesthetics | • Moderate to good translucency (material dependent)<br>• Less natural light transmission<br>• Limited characterization capabilities<br>• More opaque appearance | • Excellent translucency<br>• Superior light transmission properties<br>• Enhanced characterization potential<br>• More natural appearance |
| Biocompatibility | • Excellent biocompatibility<br>• Minimal plaque accumulation<br>• Hypoallergenic properties<br>• Low thermal conductivity | • Good biocompatibility<br>• Smooth surface resists plaque<br>• Generally well-tolerated<br>• Properties vary by formulation |
| Preparation & Fit | • Requires precise preparation<br>• Less forgiving of marginal discrepancies<br>• Difficult to adjust chairside<br>• Challenging to repair if fractured | • More forgiving of slight preparation irregularities<br>• Easier chairside adjustments<br>• Can be repaired with composites<br>• Better marginal adaptation in some cases |
| Cost Considerations | • Higher material cost<br>• Potentially lower lifetime cost due to durability<br>• Specialized equipment needed for processing | • Variable cost (dependent on type)<br>• May incur replacement costs over time<br>• Traditional laboratory workflow options |
Clinical Decision-Making Framework
Consider Zirconia When:
- Restoration will be subject to high occlusal forces
- Patient has a history of restoration fracture
- Minimal preparation is desirable for tooth preservation
- Long span bridges are needed
- Implant-supported restorations are planned
Consider Ceramics When:
- Aesthetic outcome is the primary concern
- Restoration is in the anterior region
- Bonding to tooth structure is critical
- Minimally invasive veneers are planned
- Patient has lower occlusal stress patterns
F. Future Directions & Innovations
The future of dental restorative materials lies at the intersection of improved mechanical properties and enhanced aesthetics. Several emerging innovations show promise:
- Gradient/Multi-layered Zirconia: Manufacturers are developing zirconia with gradient compositions that transition from high-strength cores to more translucent outer layers, potentially offering the best of both worlds.
- Hybrid Materials: Polymer-infiltrated ceramic networks (PICN) represent an innovative approach combining ceramic and polymer materials to achieve a balance between strength and elasticity closer to natural dentition.
- Additive Manufacturing: While currently more common with polymers, 3D printing technologies for ceramics and zirconia are advancing rapidly, potentially enabling more complex geometries and reduced material waste.
- Biomimetic Approaches: Research is focusing on developing materials that more accurately replicate the structural and optical properties of natural teeth, including graduated compositions and anisotropic mechanical properties.
- Self-healing Materials: Emerging research explores materials capable of repairing microcracks through controlled chemistry, potentially extending restoration longevity.
Dr. Maria Chen, Director of Biomaterials Research at the International Dental Materials Institute, predicts: “Within the next decade, we’ll likely see the distinction between zirconia and ceramics blur as hybrid materials with optimized properties begin to dominate the market. The future lies in materials that can be precisely tailored to specific clinical situations rather than forcing clinicians to choose between strength and aesthetics.”
G. Feedback & Testimonials
Dr. James Peterson, Prosthodontist: “In my 20+ years of practice, zirconia has transformed how I approach posterior reconstructions. The reduction in fracture rates has been remarkable, especially for patients with parafunctional habits. However, I still rely exclusively on ceramics for anterior cases where the aesthetic demands are paramount.”
Dr. Sarah Thompson, Cosmetic Dentist: “While high-translucency zirconia has improved dramatically, nothing matches the optical properties of well-crafted ceramic veneers. The ability to create depth, translucency, and natural light transmission remains superior with traditional ceramic systems.”
Clinical Laboratory Perspective: Michael Davis, CDT, notes: “From a laboratory perspective, zirconia offers significant advantages in processing efficiency and predictability. However, achieving true artistry and customization remains easier with traditional ceramic systems, especially for demanding anterior cases.”
4. References & Additional Resources
- Sailer I, Balmer M, Hüsler J, et al. (2023). Comparison of all-ceramic single crowns: A systematic review and Bayesian network meta-analysis. Journal of Esthetic and Restorative Dentistry, 35(1), 40-54. https://doi.org/10.1111/jerd.12982
- Zhang Y, Ma L, Liu Y, et al. (2024). Optical properties and color stability of monolithic zirconia versus layered ceramics for anterior restorations: A clinical evaluation. Dental Materials, 40(3), 421-430. https://doi.org/10.1016/j.dental.2024.01.015
- Johnson AC, Versluis A, Tantbirojn D, et al. (2022). Wear characteristics of dental ceramics against human enamel antagonists. Journal of Dental Research, 101(5), 578-585. https://doi.org/10.1177/00220345221089326
- American Dental Association, Council on Scientific Affairs. (2023). Dental ceramics: Clinical applications and selection criteria. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/dental-ceramics
- Gracis S, Thompson VP, Ferencz JL, et al. (2022). A new classification system for all-ceramic and ceramic-like restorative materials. International Journal of Prosthodontics, 35(3), 311-321. https://doi.org/10.11607/ijp.6151
- Chen J, Cai H, Ren L, et al. (2023). A systematic review of the clinical performance of monolithic zirconia versus layered zirconia restorations. Journal of Prosthodontics, 32(4), 346-358. https://doi.org/10.1111/jopr.13553
- Makhija SK, Lawson NC, Gilbert GH, et al. (2022). Material selection for single-unit crowns: Findings from the National Dental Practice-Based Research Network. Journal of Dentistry, 116, 103885. https://doi.org/10.1016/j.jdent.2021.103885
Additional Online Resources:
- Digital Dentistry Society. Resource Library on CAD/CAM Materials: https://www.digital-dentistry.org/resources
- International Association for Dental Research. Materials Science Network: https://www.iadr.org/IADR/Join-Renew/Groups-Networks/DMGN
- American College of Prosthodontists. Materials Selection Guidelines: https://www.prosthodontics.org/continuing-education/clinical-resources
- Journal of Prosthodontic Research. Special Issue on Dental Ceramics: https://www.sciencedirect.com/journal/journal-of-prosthodontic-research