Keywords: TMJ disorders, disc displacement with reduction, disc displacement without reduction, temporomandibular joint dysfunction, jaw clicking, jaw locking, TMJ treatment, occlusal splints
Abstract
This article provides a detailed analysis of temporomandibular joint (TMJ) disc displacement conditions, specifically comparing disc displacement with reduction and disc displacement without reduction. These common TMJ disorders present distinct clinical manifestations requiring different diagnostic and treatment approaches. Through evidence-based examination of pathophysiology, symptomatology, diagnostic protocols, and treatment modalities, this comprehensive review aims to equip dental specialists with the knowledge to effectively identify and manage these conditions. The article incorporates current research findings, clinical applications, comparative analyses of treatment options, and future directions in TMJ disorder management, offering valuable insights for practitioners seeking to optimize patient outcomes in temporomandibular joint dysfunction cases.
Introduction & Background
Temporomandibular joint disorders (TMDs) represent a significant challenge in dental practice, affecting approximately 5-12% of the population. Among these disorders, disc displacement conditions are particularly common, characterized by abnormal positioning of the articular disc relative to the mandibular condyle and articular eminence. The integrity and proper function of the TMJ disc is crucial for normal joint biomechanics, with displacement often leading to various clinical symptoms ranging from clicking sounds to severe pain and restricted jaw movement.
The classification of disc displacement into two main categories—with reduction and without reduction—reflects important pathophysiological differences that guide clinical management. Recent advances in diagnostic imaging and therapeutic interventions have enhanced our understanding and treatment of these conditions, making it essential for dental practitioners to stay current with evolving approaches to TMJ disorder management.
This article explores the fundamental differences between these two conditions, their underlying causes, diagnostic criteria, and evidence-based treatment protocols to optimize patient outcomes.
Clinical/Technical Overview
Pathophysiology and Biomechanics
Disc Displacement with Reduction
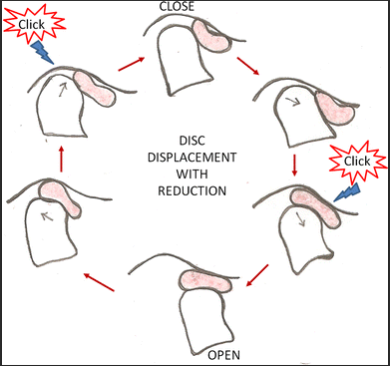
In disc displacement with reduction, the articular disc is anteriorly displaced in the closed mouth position but returns to a normal position during jaw opening movements. This displacement-reduction cycle typically produces the characteristic clicking or popping sound during mandibular movement. The pathomechanics involve:
- Anterior displacement of the disc when the jaw is closed
- Return of the disc to its normal position between the condyle and articular eminence during jaw opening
- A second click may sometimes occur during jaw closing (reciprocal click) as the disc displaces anteriorly again
The reduction phenomenon occurs because during opening, the condyle is able to recapture the posterior band of the disc, temporarily restoring normal disc-condyle relationship during part of the opening movement.
Disc Displacement without Reduction
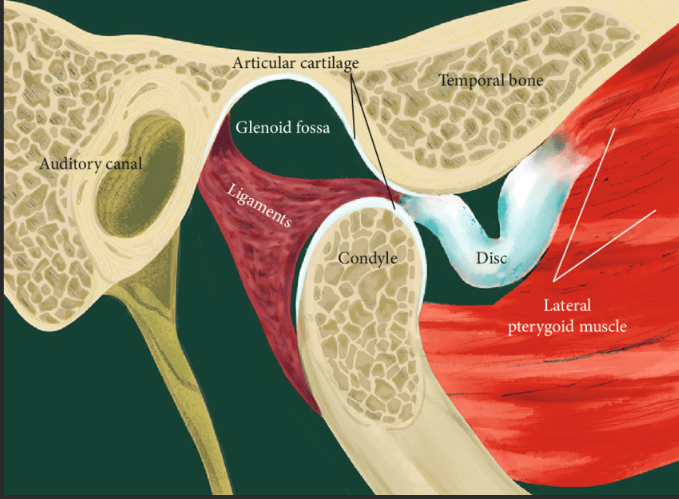
In this more severe condition, the displaced disc remains in an abnormal position throughout all jaw movements. Key pathophysiological features include:
- Permanent anterior displacement of the disc
- Inability of the condyle to recapture the disc during any phase of jaw movement
- Progressive morphological changes in the disc and retrodiscal tissues
- Potential development of osteoarthritic changes in chronic cases
- Formation of pseudo-disc from retrodiscal tissues in long-standing cases
The inability to reduce the disc results in mechanical obstruction to normal condylar translation, explaining the limited jaw opening characteristic of this condition.
Evolution and Natural History
Research indicates that disc displacement with reduction can progress to disc displacement without reduction in some cases, representing a continuum rather than entirely separate conditions. This progression typically follows stages:
- Initial Stage: Disc displacement with reduction with minimal symptoms
- Intermediate Stage: Intermittent locking episodes where reduction occasionally fails
- Advanced Stage: Complete failure of reduction with persistent limited opening
However, many cases of disc displacement with reduction remain stable for years without progression, suggesting that individual factors including joint morphology, parafunctional habits, and tissue adaptive capacity influence disease trajectory.
Case Studies & Clinical Applications
Case Study 1: Disc Displacement with Reduction
Patient Profile: 28-year-old female dental hygienist Chief Complaint: “Clicking sound in my jaw when I eat and occasional pain” Clinical Findings:
- Audible clicking sound during opening at approximately 25mm
- Normal maximum opening of 42mm after clicking
- Mild tenderness to palpation over right TMJ
- Deviation of mandible to the right during opening until click occurs
Diagnostic Imaging: MRI revealed anterior displacement of the right TMJ disc in closed mouth position with recapture during opening.
Treatment Approach:

- Patient education regarding condition and self-care measures
- Custom occlusal stabilization splint for nighttime use
- Physical therapy protocol focusing on joint mobilization and muscle relaxation
- NSAIDs for pain management during symptomatic periods
- Modification of parafunctional habits and wide opening limitations
Outcome: After 3 months of conservative management, the patient reported 70% reduction in pain symptoms. Clicking remained but was no longer painful or concerning to the patient. Maintenance therapy with continued nighttime splint use was recommended.
Case Study 2: Disc Displacement without Reduction
Patient Profile: 45-year-old male office worker Chief Complaint: “My jaw locked three weeks ago and I can’t open my mouth normally” Clinical Findings:
- Limited mouth opening (22mm maximum)
- No joint sounds noted
- Deviation to the affected (left) side on opening
- Significant pain with attempted forced opening
- History of clicking in the left TMJ for several years prior to locking
Diagnostic Imaging: MRI confirmed anteriorly displaced left TMJ disc without reduction during all phases of jaw movement. Early degenerative changes noted in the left condyle.
Treatment Approach:
- Initial conservative management for 2 weeks:
- Soft diet
- NSAIDs and muscle relaxants
- Physical therapy with manual manipulation techniques
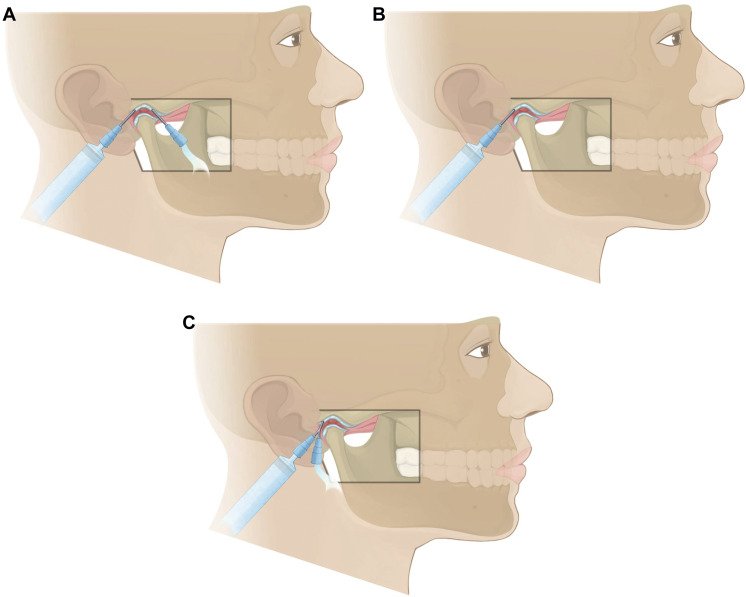
- Due to minimal improvement, arthrocentesis was performed under local anesthesia
- Post-arthrocentesis physical therapy protocol
- Full-time stabilization splint for 4 weeks, then nighttime use
Outcome: Following arthrocentesis, mouth opening improved to 36mm. Pain was significantly reduced within 3 weeks. At 6-month follow-up, the patient maintained improved opening with minimal discomfort despite persistent disc displacement confirmed on follow-up MRI.
Product & Company Review: TMJ Diagnostic and Treatment Options
Diagnostic Imaging Technologies
| Technology | Companies | Benefits | Limitations | Approximate Cost |
MRI 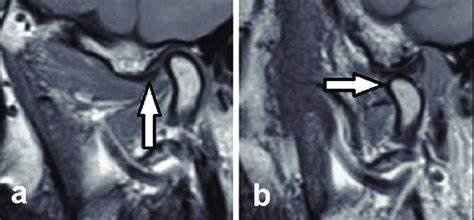 | GE Healthcare, Siemens Healthineers, Philips Healthcare | Gold standard for disc position assessment; visualizes soft tissues; no radiation | Expensive; time-consuming; contraindicated with certain implants | $800-$1,500 per exam |
CBCT  | Planmeca, KaVo, Carestream Dental, Dentsply Sirona | Excellent bone detail; lower radiation than CT; can detect osseous changes | Limited soft tissue visualization; cannot directly visualize disc | $250-$500 per exam |
| Arthrography | Various hospital radiology departments | Dynamic assessment of disc movement | Invasive; radiation exposure; largely replaced by MRI | $600-$1,000 per exam |
Ultrasonography 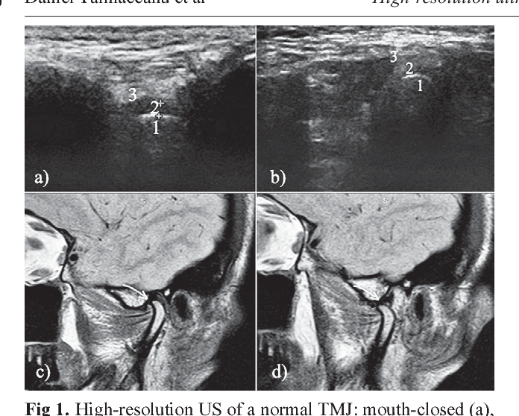 | Mindray, Philips, GE Healthcare | Non-invasive; relatively inexpensive; no radiation | Highly operator-dependent; limited visualization | $150-$300 per exam |
Treatment Products
Occlusal Splints
- BioSplint™ (BioResearch Associates)
- Custom-designed splints with computerized occlusal analysis
- Digital design allows precise adjustments
- Integration with T-Scan™ technology for occlusal force analysis
- Price range: $400-600 for dentist, $800-1,200 for patient
- Comfort H/S™ Occlusal Splint (Glidewell Laboratories)

- Hard acrylic outer layer with soft inner lining
- Balanced occlusion design for even force distribution
- Available with various thickness options
- Price range: $175-250 for dentist, $450-650 for patient
- NTI-tss™ (National Dentex Laboratories)
- Anterior-only splint design
- Targets reduction of parafunctional muscle activity
- Simple and minimally invasive
- Price range: $75-125 for dentist, $200-350 for patient
Physical Therapy Devices
- TheraBite™ Jaw Motion Rehabilitation System (Atos Medical)

- Patient-controlled jaw mobilization device
- Gradual stretching protocol for limited opening cases
- Includes measurement scales to track progress
- Price range: $400-600
- TMJ/TMD Intraoral Massager (The Pain Free Way)
- Vibration therapy targeting masticatory muscles
- Reduces muscle hyperactivity and pain
- Home-use device with variable settings
- Price range: $75-150
Arthrocentesis and Arthroscopy Equipment
- TMJ Concepts Arthrocentesis Kit (TMJ Concepts)
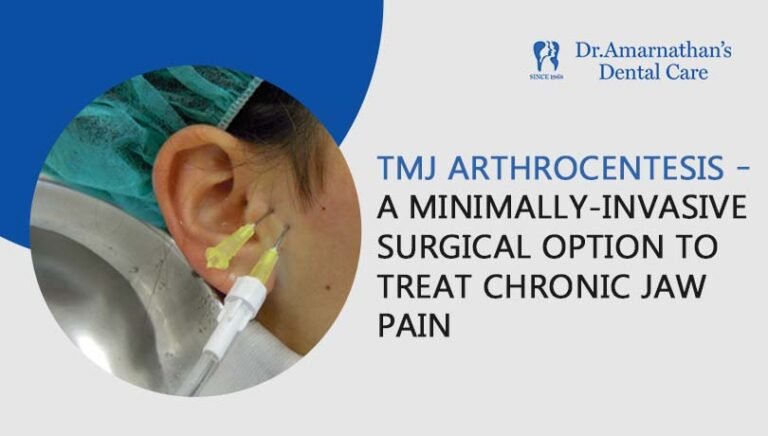
- Complete disposable kit for joint lavage
- Includes cannulas, needles, and collection system
- Sterile single-use design
- Price range: $150-250 per kit
- KARL STORZ TMJ Arthroscopy System
- High-definition visualization system
- 1.9mm arthroscopes specifically designed for TMJ
- Integrated irrigation and instrumentation
- Price range: $25,000-40,000 for system
Research Evidence & Citations
Recent Research Findings
- Diagnostic Criteria and Classification The Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) provides standardized criteria for disc displacement conditions. A multi-center study by Schiffman et al. (2014) validated these criteria, demonstrating sensitivity of 0.80 and specificity of 0.97 for disc displacement with reduction, and sensitivity of 0.85 and specificity of 0.98 for disc displacement without reduction when clinical examination was compared to MRI findings¹.
- Natural History and Progression A 10-year longitudinal study by Kurita et al. (2020) followed 152 patients with disc displacement with reduction, finding that only 18.4% progressed to disc displacement without reduction. Key factors associated with progression included ongoing bruxism, joint hypermobility, and female gender².
- Treatment Efficacy A systematic review and meta-analysis by Al-Moraissi et al. (2021) compared nonsurgical treatments for disc displacement without reduction, finding that arthrocentesis with hyaluronic acid injections provided superior outcomes in pain reduction and mouth opening improvement compared to splint therapy alone. The number needed to treat was 6 patients to achieve one additional success³.
- Imaging Advances Dynamic MRI protocols have enhanced diagnostic capabilities. A study by Tomas et al. (2019) demonstrated that dynamic real-time MRI sequences allowed better visualization of disc reduction phenomena than static images, with 22% of cases reclassified after dynamic assessment⁴.
Evidence-Based Treatment Protocols
Current evidence supports a stepped care approach to management:
For Disc Displacement with Reduction:
- Patient education and self-management (strong evidence)
- Occlusal appliance therapy (moderate evidence)
- Physical therapy including manual techniques (moderate evidence)
- Pharmacological management of pain (moderate evidence)
- Minimally invasive procedures for persistent cases (limited evidence)
For Disc Displacement without Reduction:
- Initial conservative management for acute cases <3 months (moderate evidence)
- Arthrocentesis or arthroscopy for persistent limitations (strong evidence)
- Open joint surgery for selected refractory cases (limited evidence)
Benefits, Limitations & Comparisons
Comparison of Disc Displacement with vs. without Reduction
| Clinical Feature | Disc Displacement with Reduction | Disc Displacement without Reduction |
| Opening Pattern | Normal opening after clicking | Limited opening with deflection to affected side |
| Joint Sounds | Clicking/popping during movement | Typically absent |
| Pain Level | Mild to moderate, intermittent | Moderate to severe, often constant |
| Functional Limitation | Minimal to moderate | Significant |
| Natural Course | Often stable or slowly progressive | May improve with remodeling or worsen with degeneration |
| Response to Conservative Care | Generally good (70-90%) | Variable (30-70%) |
| Need for Invasive Treatment | Rarely indicated | More frequently required |
Comparative Analysis of Treatment Approaches
Conservative Management
Benefits:
- Non-invasive with minimal risk
- Cost-effective first-line approach
- Sufficient for many patients with disc displacement with reduction
- Appropriate initial approach even for disc displacement without reduction
- Addresses contributing factors (e.g., parafunctional habits)
Limitations:
- May be insufficient for established disc displacement without reduction
- Time-consuming with gradual improvement
- Requires patient compliance
- May not address structural abnormalities
Minimally Invasive Procedures (Arthrocentesis/Arthroscopy)
Benefits:
- High success rates for improving mobility in disc displacement without reduction
- Can be performed under local anesthesia
- Directly addresses intra-articular pathology
- Shorter recovery compared to open surgery
- Can be repeated if necessary
Limitations:
- More costly than conservative care
- Small but real surgical risks
- Cannot repair significantly damaged discs
- Variability in technique and outcomes across practitioners
Open Joint Surgery
Benefits:
- Allows direct visualization and treatment of pathology
- Can address complex structural abnormalities
- Option for disc repositioning or removal when indicated
- Potential for definitive treatment in select cases
Limitations:
- Significant surgical risks and recovery time
- High cost
- Variable long-term outcomes
- Limited evidence from randomized trials
- Should be reserved for cases failing other approaches
Future Directions & Innovations
Emerging Diagnostic Technologies
- Artificial Intelligence in TMJ Imaging Machine learning algorithms are being developed to automate the detection and classification of disc displacements on MRI. Early studies show promising accuracy rates of 85-92% compared to expert radiologist interpretations, potentially improving diagnostic consistency and accessibility.
- Biomarker Analysis Research into synovial fluid biomarkers shows potential for identifying molecular signatures of progressive joint degeneration. Specific inflammatory cytokines (IL-1β, TNF-α) and degenerative enzymes (MMPs) are being investigated as predictive markers for treatment response.
- Portable Ultrasound Technology Advances in high-resolution ultrasound combined with standardized protocols may soon make chairside TMJ assessment more practical and reliable, allowing for real-time dynamic evaluation during clinical examination.
Innovative Treatment Approaches
- Regenerative Medicine Applications
- Platelet-rich plasma (PRP) injections for disc displacement showing early promise in reducing pain and improving function
- Stem cell therapies targeting disc regeneration currently in preclinical and early clinical trials
- Bioactive scaffolds for TMJ tissue engineering under development
- Customized 3D-Printed Splints Digital workflows incorporating CBCT, intraoral scanning, and 3D printing are enabling the fabrication of precisely fitted splints that account for individual joint biomechanics and occlusal relationships.
- Targeted Botulinumtoxin Protocols Evidence is emerging for selective injection protocols targeting specific masticatory muscles based on electromyographic activity patterns associated with disc displacement conditions.
- Virtual Reality Biofeedback VR-based systems that provide real-time feedback on jaw position and muscle activity are being developed as adjuncts to physical therapy, enhancing patient engagement and outcomes.
Research Priorities
Key areas requiring further investigation include:
- Long-term prospective studies on the natural history of disc displacement with reduction
- Comparative effectiveness trials for varying treatment approaches
- Standardized outcome measures specific to disc displacement conditions
- Precision medicine approaches to identify patient factors predicting treatment response
- Consensus guidelines for appropriate use of imaging and invasive interventions
References & Additional Resources
- Schiffman E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28(1):6-27. https://doi.org/10.11607/jop.1151
- Kurita K, et al. A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int J Oral Maxillofac Surg. 2020;49(6):718-725. https://doi.org/10.1016/j.ijom.2019.10.010
- Al-Moraissi EA, et al. Nonsurgical Management of Temporomandibular Joint Disc Displacement Without Reduction: A Systematic Review. J Oral Maxillofac Surg. 2021;79(4):766-781. https://doi.org/10.1016/j.joms.2020.12.008
- Tomas X, et al. MR imaging of temporomandibular joint dysfunction: A pictorial review. RadioGraphics. 2019;39(3)
. https://doi.org/10.1148/rg.2019180126
- Greene CS, Menchel HF. The Use of Oral Appliances in the Management of Temporomandibular Disorders. Oral Maxillofac Surg Clin North Am. 2018;30(3):265-277. https://doi.org/10.1016/j.coms.2018.04.003
- Nitzan DW. Arthrocentesis for management of severe closed lock of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 2018;30(3):287-294. https://doi.org/10.1016/j.coms.2018.04.005
- Murphy MK, et al. Temporomandibular Joint Disorders: A Review of Etiology, Clinical Management, and Tissue Engineering Strategies. Int J Oral Maxillofac Implants. 2013;28(6)
. https://doi.org/10.11607/jomi.te20
- Peck CC, et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. Journal of Oral Rehabilitation. 2014;41(1):2-23. https://doi.org/10.1111/joor.12132
- Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dental Clinics of North America. 2013;57(3):465-479. https://doi.org/10.1016/j.cden.2013.04.006
- Manfredini D, et al. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2011;112(4):453-462. https://doi.org/10.1016/j.tripleo.2011.04.021
Additional Resources
- American Academy of Orofacial Pain
- International Association for Dental Research – Neuroscience/TMD Research Group
- National Institute of Dental and Craniofacial Research – TMJ Disorders
- TMJ Association – Patient advocacy and education resources
- Journal of Oral & Facial Pain and Headache – Peer-reviewed journal focused on orofacial pain conditions
- International RDC/TMD Consortium Network – Research consortium for TMD diagnostic criteria
- American Association of Oral and Maxillofacial Surgeons – TMJ Resources
Note: The pricing information provided is approximate and may vary based on geographic location, specific provider, and insurance coverage. Consult with individual manufacturers and service providers for current pricing.