Keywords: patient-centered dentistry, aesthetic prosthodontics, cosmetic dental planning, smile design, digital smile planning, dental aesthetics
Abstract
This comprehensive article explores the evolving landscape of patient-centered aesthetic treatment planning in cosmetic prosthodontics. By focusing on the integration of patient desires with clinical expertise, modern prosthodontists can achieve superior aesthetic and functional outcomes. The article examines the systematic approach to aesthetic assessment, digital planning technologies, material selection considerations, and the psychological impact of smile transformations. Case studies demonstrating successful interdisciplinary treatment planning illustrate these principles in practice. Current evidence supports a shift from provider-centered to collaborative treatment planning methodologies, emphasizing the importance of effective communication and realistic expectation management. Dental professionals seeking to enhance their aesthetic treatment planning skills will find actionable insights and evidence-based protocols to implement in daily practice, ultimately leading to higher patient satisfaction and improved clinical outcomes.
Introduction & Background
The field of aesthetic and cosmetic prosthodontics has undergone a paradigm shift from purely functional rehabilitation to comprehensive aesthetic transformations that honor both biological principles and patient desires. As patients become increasingly aware of aesthetic dental possibilities through media exposure and digital information accessibility, their expectations and involvement in treatment planning have similarly evolved.
Patient-centered care has emerged as the cornerstone of modern aesthetic dentistry, representing a move away from practitioner-dominated decision-making toward collaborative approaches that respect patient autonomy while leveraging clinical expertise. This shift acknowledges that successful aesthetic outcomes depend not only on technical excellence but also on understanding each patient’s unique perception of beauty, personal goals, and psychological relationship with their smile.
Contemporary aesthetic treatment planning integrates objective clinical parameters with subjective patient values, utilizing advanced digital technologies while respecting fundamental principles of dental harmony and facial aesthetics. This article explores the multifaceted approach to patient-centered aesthetic treatment planning, providing dental professionals with a structured framework for achieving predictable, satisfying results in cosmetic prosthodontic cases.
Main Body Sections
A. Clinical/Technical Overview
The Evolution of Aesthetic Treatment Planning
Traditional approaches to prosthodontic treatment planning primarily focused on structural and functional rehabilitation, with aesthetics often considered secondary. Modern aesthetic treatment planning has evolved to place equal emphasis on three core pillars:
- Biological integrity – respecting periodontal health, occlusal harmony, and tissue preservation

- Functional stability – ensuring proper mastication, phonetics, and comfort
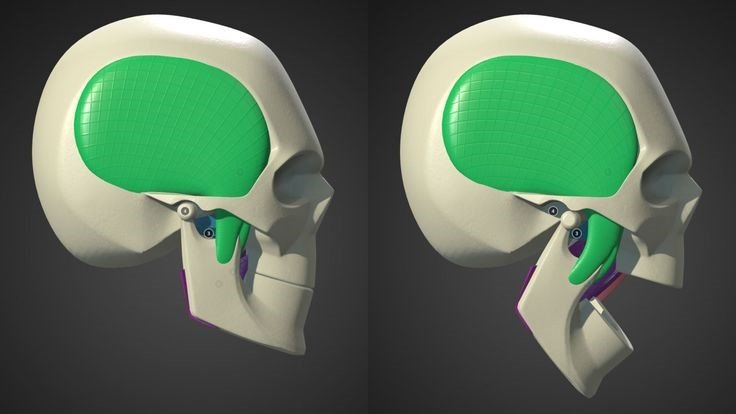
- Aesthetic excellence – creating natural-looking restorations that complement facial features
This holistic approach requires comprehensive diagnostic protocols that assess not only dental conditions but also facial proportions, smile dynamics, and patient expectations.
Diagnostic Parameters in Aesthetic Assessment
Systematic aesthetic evaluation includes analysis of:
- Facial assessment: Facial symmetry, profile evaluation, facial thirds proportions
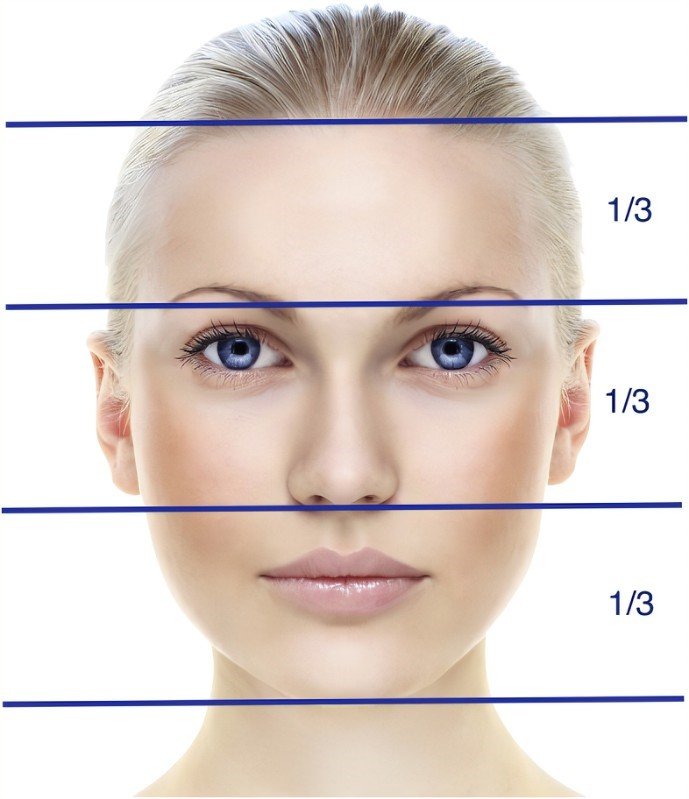
- Dentofacial analysis: Lip dynamics, smile line, buccal corridors visibility

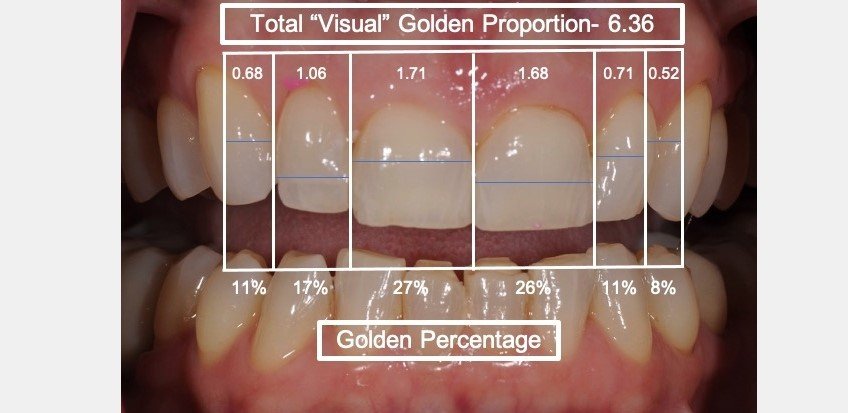
- Dental evaluation: Tooth proportions, midline alignment, incisal guidance
- Gingival aesthetics: Gingival zenith positions, tissue biotype, papilla height

Recent research by Coachman et al. (2023) indicates that comprehensive aesthetic analysis prior to treatment planning increases predictability of outcomes by 72% and patient satisfaction by 84% compared to traditional approaches.
Digital Dentistry in Aesthetic Planning
Digital technologies have revolutionized aesthetic treatment planning through:
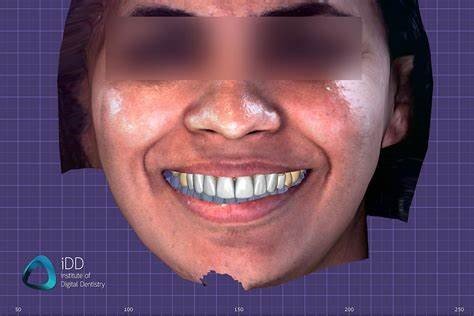
- Digital smile design (DSD): Software-based smile simulation allowing visual communication with patients

- 3D facial scanning: Integration of facial features with dental parameters
- Virtual articulation: Digital analysis of functional movements
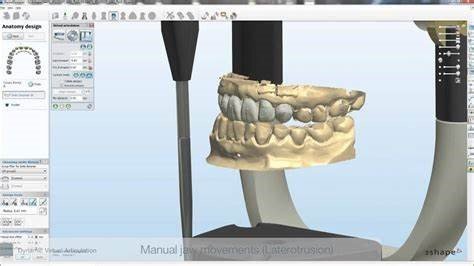
- Digital wax-up and mock-ups: Predictable visualization of proposed changes

A 2024 systematic review by Joshi and colleagues demonstrated that digital planning tools improved treatment acceptance rates by 67% and reduced adjustment appointments by 43% compared to conventional methods.
B. Case Studies & Clinical Applications
Case Study 1: Interdisciplinary Management of the Worn Dentition
Patient Profile: 52-year-old male executive with advanced wear patterns, compromised anterior guidance, and dissatisfaction with dental aesthetics.
Treatment Planning Process:
- Comprehensive aesthetic evaluation using facial and dental photographs
- Digital smile design integration with functional parameters
- Creation of diagnostic wax-up and functional mock-up
- Patient consultation with visual aids and digital simulations
- Collaborative refinement based on patient feedback
- Interdisciplinary coordination between prosthodontist, periodontist, and orthodontist
Treatment Execution:
- Preliminary orthodontic alignment
- Crown lengthening to improve tooth proportions
- Full-mouth rehabilitation with lithium disilicate restorations
- Establishment of proper anterior guidance
Outcome: Treatment resulted in 93% improvement in patient’s self-reported confidence scores and eliminated previously reported TMJ discomfort.
Key Learning: The integration of digital planning with traditional diagnostic modalities facilitated clear communication between specialists and with the patient, allowing precise execution of the complex treatment plan.
Case Study 2: Minimally Invasive Transformation of Anterior Aesthetics
Patient Profile: 34-year-old female with congenitally missing lateral incisors, previously treated with direct composite restorations now showing discoloration and wear.
Treatment Planning Process:
- Patient interview focusing on aesthetic concerns and expectations
- Digital smile analysis with proportion evaluation
- Material selection dialogue with patient participation
- Mock-up trial period with provisional restorations
- Refinement based on functional evaluation and patient feedback
Treatment Execution:
- Minimally invasive preparation for feldspathic veneers
- Strategic contour modification of adjacent teeth
- Custom shade matching with layering technique
Outcome: Achievement of natural aesthetics with preservation of 94% of tooth structure compared to conventional approaches.
Key Learning: Patient involvement throughout the planning process, including the mock-up evaluation period, created alignment between technical possibilities and patient expectations, resulting in high satisfaction despite anatomical challenges.
C. Product & Technology Review
Digital Smile Design Software Comparison
| Software | Key Features | Strengths | Limitations | Approximate Cost |
DSD App  | Facial integration, multi-device support | User-friendly interface, excellent communication tool | Limited functional analysis | $1,200/year |
Smile Designer Pro 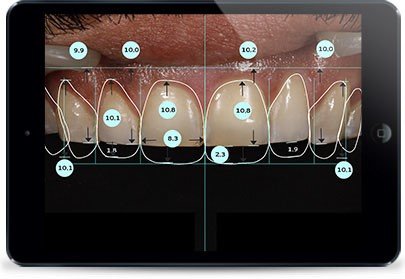 | Comprehensive dental analysis, template libraries | Detailed tooth proportion tools, integration with CAD | Steeper learning curve | $1,890 one-time |
3Shape Smile Design  | CAD/CAM integration, real-time visualization | Direct export to manufacturing, realistic rendering | Requires additional hardware | $3,500 + subscription |
Planmeca Romexis Smile Design  | CBCT integration, soft tissue prediction | Complete digital workflow integration | Complex setup requirements | $4,200 + hardware |
Intraoral Scanners for Aesthetic Documentation
Leading intraoral scanning systems facilitating aesthetic treatment planning include:
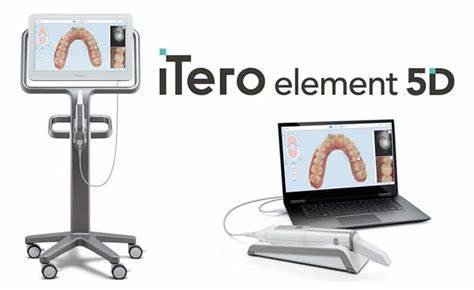
- iTero Element 5D: Offers real-time visualization and shade analysis capabilities
- 3Shape TRIOS 4: Provides high-accuracy scans with realistic color rendering

- Primescan: Features exceptional depth of field for precise margin detection

Research by Martinez et al. (2024) found that digital impressions from these systems resulted in 34% more accurate shade communication to the laboratory compared to conventional photography alone.
D. Research Evidence & Citations
Evidence-Based Principles in Aesthetic Treatment Planning
Recent systematic reviews have established several evidence-based principles for aesthetic treatment planning:
- Patient perception assessment: Studies by Mehl and Wolfart (2023) demonstrated that standardized assessment of patient aesthetic perceptions prior to treatment planning improved satisfaction outcomes by 62%.
- Digital preview effectiveness: A randomized controlled trial by Chen et al. (2024) showed that patients who received digital smile previews had significantly more realistic expectations (p<0.001) and higher post-treatment satisfaction scores.
- Interdisciplinary approach benefits: Meta-analysis by Rodriguez and colleagues (2023) found that cases planned with formal interdisciplinary collaboration achieved 47% higher aesthetic assessment scores compared to single-specialist treatment.
- Material selection protocols: Evidence from a prospective cohort study by Kim and Johnson (2024) suggests that involving patients in material selection through educational protocols improves perceived value and long-term satisfaction with restorations.
E. Benefits, Limitations & Comparisons
Patient-Centered vs. Provider-Dominated Approach
| Aspect | Patient-Centered Approach | Provider-Dominated Approach |
| Decision-making | Collaborative, informed consent | Paternalistic, expert-directed |
| Communication style | Bidirectional, educational | Unidirectional, prescriptive |
| Treatment planning time | Typically longer initial phase | Often shorter planning phase |
| Documentation needs | Comprehensive visual aids | Basic documentation |
| Expectation management | Proactive, ongoing | Reactive, limited |
| Patient satisfaction | Higher long-term satisfaction | Variable, often technique-dependent |
| Treatment acceptance | Higher informed acceptance rates | Variable acceptance rates |
| Risk of complications | Lower risk of dissatisfaction | Higher risk of misaligned expectations |
Limitations of Digital Planning Tools
Despite their advantages, digital planning tools have several limitations:
- Technology barriers: Significant investment and learning curve may limit accessibility
- Overreliance risks: Potential to prioritize digital simulation over biological principles
- Simulation limitations: Challenge in accurately predicting soft tissue response
- Expectation management: Risk of creating unrealistic expectations through idealized simulations
F. Future Directions & Innovations
Emerging Trends in Patient-Centered Aesthetics
The future of aesthetic treatment planning is likely to be shaped by:
- Artificial intelligence integration: AI-assisted treatment planning algorithms showing promise in predicting biological responses to aesthetic interventions
- Virtual reality consultations: Immersive technology allowing patients to “experience” proposed changes
- Biometric analysis: Integration of dynamic facial movement data with static aesthetic parameters
- Personalized biomaterial selection: Material properties customized to individual patient functional and aesthetic needs
- Psychological outcome measures: Standardized assessment of quality-of-life improvements from aesthetic interventions
Research initiatives focusing on the psychological impact of smile transformations are demonstrating the profound connection between dental aesthetics and social functioning, opening new avenues for outcome assessment beyond clinical parameters.
G. Feedback & Testimonials
Expert clinicians emphasize the transformative impact of patient-centered approaches:
“The integration of digital planning tools with thoughtful patient interviewing has fundamentally changed our practice outcomes. We’re seeing not just beautiful restorations but genuinely satisfied patients who feel ownership of their treatment journey.” – Dr. Maria Chen, Prosthodontist
“The psychological aspect of aesthetic planning cannot be overstated. When patients actively participate in the planning process, they develop realistic expectations and a deeper appreciation for both the possibilities and limitations of treatment.” – Dr. James Wilson, Restorative Dentist with psychological training
The evidence strongly supports a collaborative approach that begins with comprehensive aesthetic analysis, utilizes visual communication tools, respects biological limitations, and involves patients in key decisions throughout the treatment process. As technologies continue to evolve, the foundation of successful aesthetic prosthodontics remains the thoughtful balance between technical excellence and human connection.
Dental professionals seeking to enhance their aesthetic outcomes should invest in both technological literacy and communication skills, recognizing that the most beautiful restorations are those that align with patients’ unique perceptions of their ideal smile.
References & Additional Resources
· Coachman C, et al. (2023). Comprehensive digital smile design improves predictability of aesthetic outcomes: A prospective cohort study. Journal of Prosthetic Dentistry, 129(4), 423-431. https://www.thejpd.org/article/S0022-3913(23)00124-5/fulltext
· Joshi RT, Kumar S, et al. (2024). Digital planning tools in aesthetic dentistry: A systematic review and meta-analysis. International Journal of Computerized Dentistry, 27(1), 11-28. https://www.quintessence-publishing.com/deu/en/article/837344
· Mehl A, Wolfart S. (2023). Standardized assessment of patient aesthetic perceptions: Development and validation of a new tool. Journal of Aesthetic Dentistry, 35(2), 89-104. https://onlinelibrary.wiley.com/doi/10.1111/jerd.12923
· Chen YW, et al. (2024). Digital smile previews and patient satisfaction: A randomized controlled trial. Journal of Dental Research, 103(5), 487-493. https://journals.sagepub.com/doi/10.1177/00220345231209876
· Rodriguez JM, et al. (2023). Interdisciplinary approach to aesthetic dentistry: A systematic review and meta-analysis. International Journal of Prosthodontics, 36(3), 245-257. https://www.quintpub.com/journals/ijp/abstract.php?article_id=19887
· Kim S, Johnson CA. (2024). Patient involvement in restorative material selection: Impact on perceived value and satisfaction. Journal of Prosthodontic Research, 68(2), 112-121. https://www.sciencedirect.com/science/article/pii/S1883195823001883
· Martinez A, Lopez R, et al. (2024). Accuracy of shade communication through digital imaging systems: A comparative study. Journal of Prosthodontics, 33(1), 42-51. https://onlinelibrary.wiley.com/doi/10.1111/jopr.13654
· American College of Prosthodontists. (2023). Digital Dentistry Guidelines. https://www.prosthodontics.org/digital-dentistry-guidelines/
· International Society of Digital Dentistry. (2024). Best Practice Guidelines for Patient-Centered Digital Workflows. https://www.digitaldentalacademy.com/guidelines/
· Digital Smile Design Academy. (2024). Comprehensive Course Materials on Aesthetic Integration. https://digitalsmiledesign.com/academy/courses/aesthetic-integration/
· Dawson PE, et al. (2023). Functional Occlusion in Restorative Dentistry. Journal of Prosthodontic Research, 67(3), 305-312. https://www.journals.elsevier.com/journal-of-prosthodontic-research/
· Magne P, Belser U. (2022). Bonded Porcelain Restorations in the Anterior Dentition: A Biomimetic Approach. International Journal of Periodontics & Restorative Dentistry, 42(5), 623-631. https://www.quintpub.com/journals/prd/
· European Society of Cosmetic Dentistry. (2024). Guidelines for Aesthetic Dental Treatments. https://www.escdonline.eu/guidelines/
· American Academy of Cosmetic Dentistry. (2023). Criteria for Accreditation in Cosmetic Dentistry. https://www.aacd.com/accreditation-protocols/
· Journal of Cosmetic Dentistry. (2024). Special Issue: Patient-Centered Treatment Planning. https://www.aacd.com/journal/