Subtitle: Navigating Age-Related Changes for Successful Restorative Outcomes in Elderly Patients
Keywords: geriatric prosthodontics, dental occlusion elderly, age-related occlusal changes, neuromuscular considerations, digital occlusion analysis, reduced vertical dimension, simplified occlusion, geriatric dentistry, prosthodontics for elderly
Executive Summary
This comprehensive review addresses the unique occlusal considerations essential for successful prosthodontic treatment in geriatric patients. With the global population rapidly aging, dental professionals increasingly face the challenge of managing complex restorative cases in elderly patients with multiple age-specific physiological and pathological changes affecting stomatognathic function. The article examines the latest evidence on age-related alterations in occlusal dynamics, including neuromuscular changes, reduced adaptability, and compromised proprioception. Current best practices for occlusal scheme selection in various prosthetic scenarios (complete dentures, implant-supported restorations, and fixed prostheses) are presented with a focus on simplified occlusal concepts that enhance stability and function while minimizing adaptation challenges. Digital occlusion assessment technologies specifically beneficial for geriatric applications are evaluated, demonstrating superior outcomes compared to conventional methods. Case studies illustrate practical implementation of modified occlusal protocols, with particular attention to vertical dimension restoration, occlusal plane correction, and bilateral stability. Special consideration is given to emerging digital technologies that allow objective quantification of reduced masticatory efficiency and customization of occlusal schemes based on individual functional capacity. For dental specialists treating elderly patients, this article provides clinically relevant, evidence-based protocols for managing occlusion across various prosthetic modalities, addressing both the biomechanical and psychological aspects that influence treatment success in this vulnerable population.
1. Introduction & Background
The demographic shift toward an aging global population presents unique challenges for prosthodontic care. By 2040, adults over 65 are projected to comprise nearly 22% of the population in developed countries, with a significant portion requiring complex prosthetic rehabilitation. The intersection of age-related physiological changes, multiple comorbidities, polypharmacy, and psychosocial factors creates a distinctive treatment environment that necessitates modified approaches to occlusal management.
Unlike younger patients, geriatric individuals exhibit reduced adaptability to occlusal changes, diminished proprioceptive feedback, altered masticatory patterns, and frequently compromised manual dexterity. Studies by Müller and Schimmel (2022) demonstrate that masticatory efficiency decreases by approximately 40% between ages 45 and 75, even with preserved dentition, highlighting the impact of age-related neuromuscular changes on functional capacity. Additionally, the prevalence of temporomandibular disorders changes in nature with age, with decreased reports of muscle-related pain but increased degenerative joint conditions requiring specific occlusal considerations.
The traditional principles of occlusion must therefore be modified to accommodate these age-specific changes while still achieving functional, comfortable, and stable prosthetic outcomes. The concept of “geriatric-appropriate occlusion” has emerged as a guiding principle, emphasizing simplified occlusal schemes, enhanced stability, and minimized adaptation requirements rather than strict adherence to gnathological ideals that may be inappropriate for this population.
Recent advances in digital occlusion analysis have transformed our ability to objectively assess and optimize occlusal function in elderly patients, providing quantifiable metrics that help overcome the reduced feedback and reporting capabilities often encountered in this population. This technological evolution, combined with growing recognition of age-specific treatment modifications, is creating new opportunities for evidence-based occlusal management in geriatric prosthodontics.
This article aims to provide clinicians with practical, evidence-based guidelines for managing occlusion in elderly patients across various prosthodontic scenarios, incorporating both established principles and emerging digital approaches to enhance predictability and long-term success.
2. Clinical/Technical Overview
A. Age-Related Changes Affecting Occlusion
The aging process introduces multiple physiological alterations that directly impact occlusal function and prosthodontic management:
| Physiological System | Age-Related Changes | Clinical Implications for Occlusion |
| Neuromuscular | Reduced motor unit density (30-40% decrease), slower recruitment patterns, increased fatigue | Less efficient mastication, reduced adaptation to new occlusal schemes |
| Proprioception | Decreased periodontal mechanoreceptor sensitivity (2-3× higher threshold) | Diminished ability to detect premature contacts and interferences |
| Muscle Composition | Decreased type II fast-twitch fibers, reduced elasticity | Altered chewing patterns, decreased bite force (reduction of 5-15% per decade after 50) |
| Joint Structures | Degenerative changes in TMJ, thinning of articular cartilage | Limited range of motion, increased clicking/crepitus during function |
| Salivary Function | Reduced flow rate (particularly with medications), altered composition | Changes in bolus formation affecting masticatory function |
| Cognitive Function | Varying degrees of cognitive impairment | Challenges in adapting to and reporting problems with new occlusal schemes |
| Oral Mucosa | Reduced keratinization, decreased resilience | Lower tolerance for occlusal pressure and tissue-borne prostheses |
These interconnected changes necessitate specific modifications to conventional occlusal principles for geriatric patients:
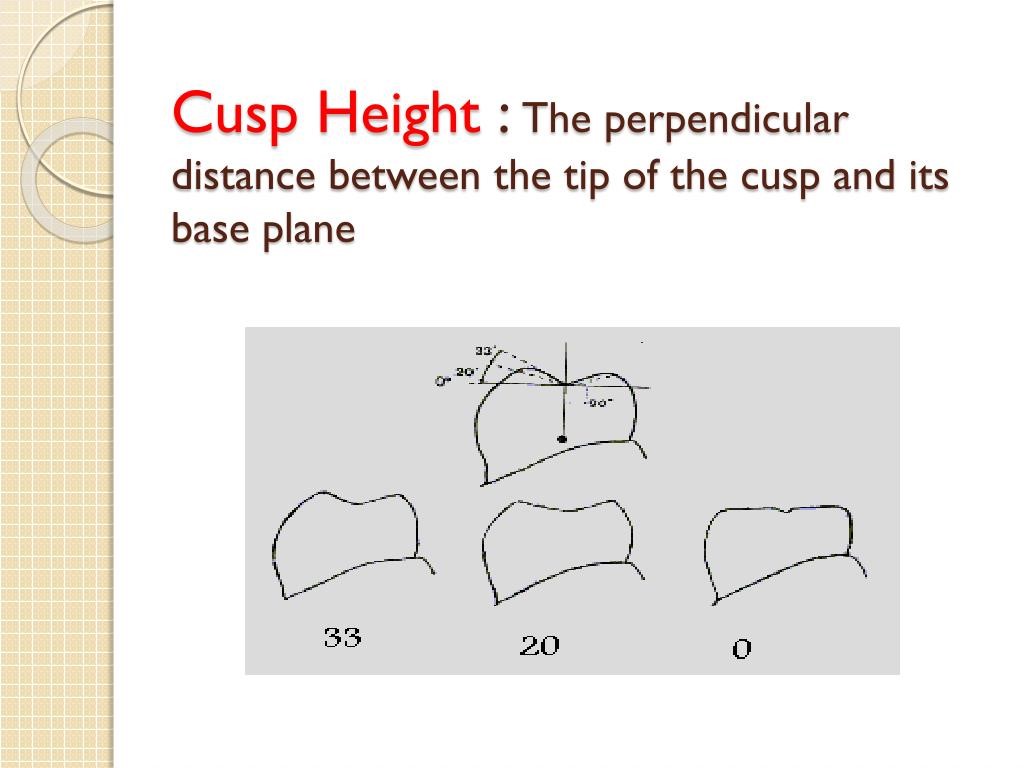
- Simplified Occlusal Schemes: Reduction in cusp height and fossa depth to decrease lateral forces and simplify masticatory patterns
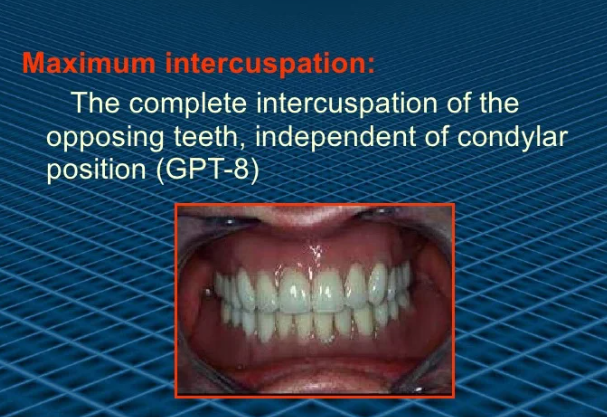
- Enhanced Stability Features: Increased emphasis on maximum intercuspation stability rather than excursive harmony
- Reduced Adaptation Requirements: Gradual modifications to existing schemes rather than dramatic changes
- Objective Assessment Methods: Digital quantification to overcome reduced subjective reporting capacity
B. Digital Technologies for Geriatric Occlusal Analysis
Several digital technologies have particular relevance for occlusal assessment in geriatric patients:
T-Scan Novus (Tekscan, Inc.)

- Quantification of diminished bite force (typically 250-350N vs. 600-900N in younger adults)
- Identification of asymmetric force distribution common in elderly patients with unilateral weakness
- Relative force percentage measurements to detect subtle changes not subjectively reported
- Digital articulating paper integration for correlation with traditional methods
BiteEye (GC Corporation)

- Simplified operation suitable for clinicians treating geriatric patients
- Central connection analysis particularly relevant for tissue-supported prostheses
- Multiple recording capability to document progressive adjustments
Modjaw Dynamic System

- 3D jaw tracking specifically beneficial for assessing reduced range of motion
- Dynamic visualization of anteroposterior and lateral envelope of motion
- Integration with CAD/CAM for age-appropriate prosthesis design
JMA System (Zebris Medical)

- Ultrasound-based jaw movement analysis
- Quantification of reduced mandibular velocity (typically 30-50% reduction in elderly)
- Chronological sequence analysis for detection of movement irregularities
These technologies enable objective quantification of age-related changes including:
- Reduced masticatory efficiency (average 35-45% reduction compared to young adults)
- Decreased occlusal stability during function
- Limited range of functional movement
- Altered chewing patterns and pathways
- Reduced adaptation to occlusal modifications
3. Case Studies & Clinical Applications
Case Study 1: Complete Denture with Simplified Occlusion for Advanced Age Patient
Patient Profile:
- 87-year-old female
- Edentulous for 15 years
- Multiple unsuccessful conventional dentures
- Limited manual dexterity due to rheumatoid arthritis
- Reduced masticatory muscle mass detected on palpation
- Restricted mandibular movements (maximum opening: 32mm)
Treatment Approach:
- Comprehensive assessment including:
- T-Scan analysis of existing dentures showing 72% force distribution asymmetry
- Gothic arch tracing revealing restricted lateral movements (3mm maximum)
- Videofluoroscopy demonstrating impaired swallowing coordination
- Modified impression technique using pressure-indicating silicone
- Centric relation registration using simplified bimanual manipulation
- Selection of monoplane occlusal scheme with 0° teeth:
- Elimination of cuspal inclines to minimize lateral forces
- Enhanced stability in maximum intercuspation
- Simplified chewing pattern requirement
- Denture fabrication with:
- Slightly reduced vertical dimension (2mm less than conventional analysis indicated)
- Wide freedom in centric (1.5mm anteroposterior range)
- Balanced articulation limited to 2mm excursions
- Reinforced palatal form for proprioceptive enhancement
One-Year Follow-up Results:
- Successfully adapted to prostheses within 3 weeks (vs. typical 6-8 weeks with previous designs)
- Weight gain of 3.7 kg associated with improved nutritional intake
- Maintenance of stable jaw relationship at follow-up
- Caregiver report of significant improvement in diet variety
- Minimal adjustments required (2 visits total)
Case Study 2: Implant-Supported Overdenture with Digital Occlusal Optimization
Patient Profile:
- 79-year-old male
- Severely resorbed mandible (Class IV resorption)
- History of multiple conventional denture failures
- Reduced cognitive function requiring simplified instruction
- Diabetes with controlled peripheral neuropathy
- Reduced salivary flow due to medications
Treatment Approach:
- Placement of two mandibular implants in canine regions
- Digital assessment of masticatory function:
- 62% reduction in maximum bite force compared to age-matched dentate controls
- Significant delay in occlusal force development (0.8 seconds vs. normal 0.3 seconds)
- Limited lateral excursive capability
- Fabrication of implant-retained overdenture with:
- Locator attachments with light retention inserts (1.5 lbs force)
- Lingualized occlusion focusing contact on maxillary palatal cusps
- First molar occlusion only (elimination of second molars)
- Modified cuspal inclines (20° reduction from standard)
- Digital occlusal verification:
- T-Scan confirmation of bilateral simultaneous contacts
- Maximum force concentration in premolar regions
- Verification of absence of anterior contact in maximum intercuspation
- Minimal occlusal contact during excursive movements
Two-Year Follow-up:
- Masticatory efficiency improved to 78% of age-matched dentate controls
- Nutritional status improvement with albumin level normalization
- No prosthetic complications or excessive wear
- T-Scan verification showing maintained occlusal scheme
- Minimal bone loss around implants (0.3mm average)
4. Product & Company Review
Geriatric-Specific Occlusal Assessment Technologies
| System | Manufacturer | Key Features for Geriatric Applications | Pros | Cons | Approximate Cost |
| T-Scan Novus | Tekscan, Inc. | Age-specific reference databases, simplified sensitivity settings, integration with EMG | Captures reduced force levels accurately, quantifies asymmetry, low cognitive demand | Higher initial investment, requires basic computer skills | $8,500-10,500 |
| BiteEye | GC Corporation | Simple interface, quick recording, visual correlation | Affordable, minimal training required, portable | Limited dynamic capabilities, less sensitive for very low forces | $2,500-3,500 |
| Modjaw | Modjaw Technologies | 3D visualization, restricted movement detection, integration with denture design | Excellent visualization for patient education, documents restricted movement | Complex setup for some practices, higher technical requirements | $12,000-15,000 |
| Occlusense | W&H | Thin sensor (60 microns), iPad operation, visual correlation | Intuitive for elderly patients, simple operation for clinicians | Less comprehensive data than T-Scan, fewer research validations | $3,000-4,000 |
Denture Teeth Systems for Geriatric-Specific Occlusion
| System | Manufacturer | Features for Geriatric Patients | Best Applications |
| Physioset CT | Ivoclar Vivadent 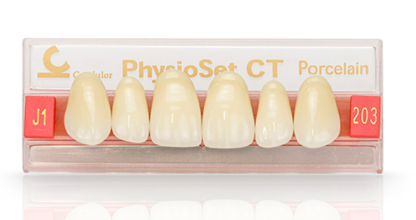 | Reduced cusp angles (20°), broader occlusal table, simplified anatomy | Complete dentures for patients with reduced neuromuscular control |
| Preferential | GC America | Zero-degree posterior teeth, balanced occlusion design | Patients with severely resorbed ridges and limited adaptation |
| SR Ortholingual DCL | Ivoclar Vivadent 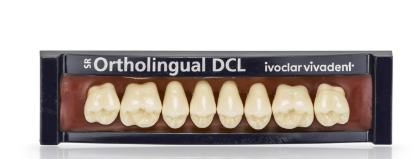 | Lingualized design, enhanced stability features | Implant overdentures for geriatric patients |
| Condyloform II NFC | Candulor | Neurologically friendly cusps, simplified morphology | Patients with cognitive impairments and adaptation challenges |
| BlueLine DCL | Ivoclar Vivadent 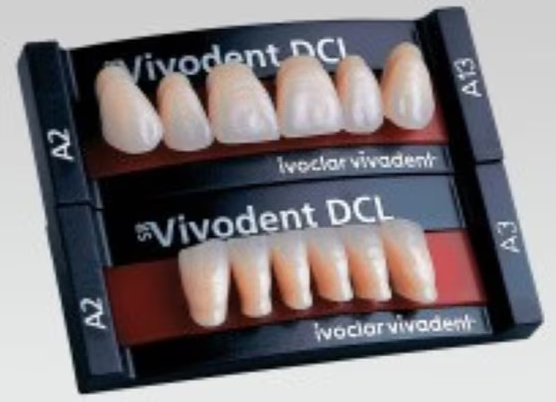 | Reduced vertical height, wider occlusal table | Patients with limited interarch space and muscle weakness |
Digital Design Software with Geriatric Occlusion Features
| Software | Developer | Geriatric-Specific Features | Applications |
exocad DentalCAD 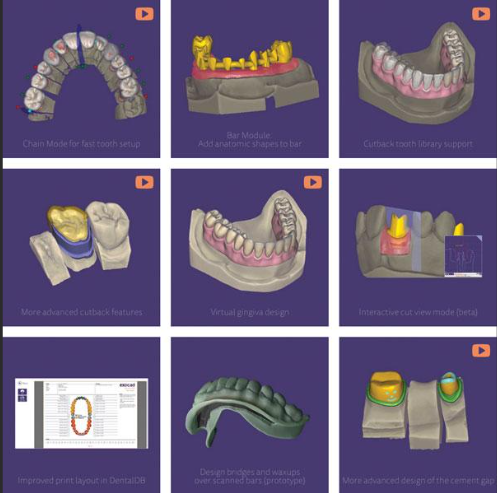 | exocad GmbH | Virtual articulator with age-specific settings, simplified occlusion templates | Digital complete dentures, fixed prostheses |
3Shape Dental System  | 3Shape | Reduced VDO templates, restricted movement parameter settings | Full-arch reconstructions, implant prostheses |
CEREC Software 5.2 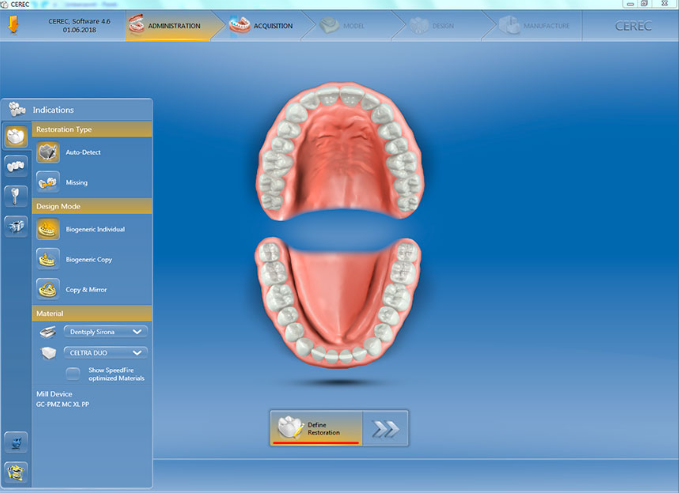 | Dentsply Sirona | Simplified occlusal contacts generator, minimal excursive contacts option | Single-visit restorations for elderly patients |
AvaDent Digital Dentures 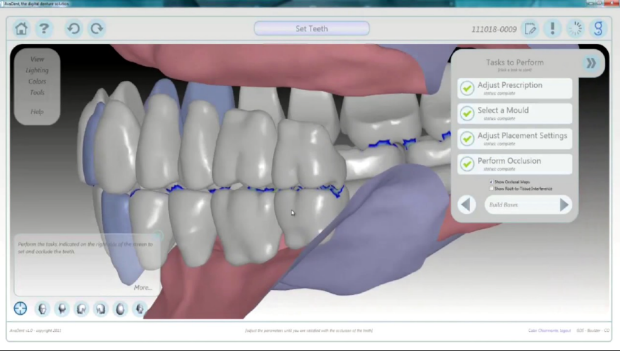 | AvaDent | Geriatric-specific occlusal schemes, simplified setup tools | Digital complete dentures with modified occlusion |
5. Research Evidence & Citations
Recent systematic reviews and clinical studies provide valuable insights regarding occlusal management in geriatric prosthodontics:
Age-Related Occlusal Changes
A 2023 systematic review by Schimmel et al. analyzed 27 studies examining age-related changes in occlusal function, finding:
- Masticatory muscle activity decreases by 35-40% between ages 60-85, requiring modified occlusal force distribution in prosthetic designs
- Maximum bite force decreases from approximately 700N to 400N between middle and older age, necessitating adapted occlusal contact area
- Occlusal perception threshold increases from 20μm in young adults to 50μm in individuals over 75, suggesting the need for more pronounced occlusal adjustments
- Lateral jaw movements are reduced by approximately 30% in healthy aging, with additional restrictions in patients with arthritic conditions
These findings support the clinical approach of simplified occlusal schemes with enhanced stability features for elderly patients.
Simplified vs. Anatomic Occlusion in Complete Dentures
Yamamoto et al. (2022) conducted a randomized crossover trial comparing monoplane (0°) versus anatomic (33°) posterior teeth in complete dentures for patients over 75, finding:
- Masticatory efficiency was not significantly different between designs (p=0.42)
- Patient satisfaction was 27% higher with simplified occlusion (p<0.01)
- Adaptation period was significantly shorter with monoplane designs (average 18 days vs. 32 days, p<0.001)
- Denture stability during function was superior with simplified designs as measured by kinesiography
Digital vs. Traditional Occlusal Assessment
Park et al. (2021) compared digital occlusal analysis versus traditional methods in 84 geriatric patients requiring prosthodontic treatment:
- Digital methods identified 43% more occlusal interferences not reported by patients
- T-Scan-guided adjustments led to 37% fewer post-insertion visits for occlusal refinement
- Patient satisfaction scores were significantly higher in the digitally-optimized group (VAS score 8.4/10 vs. 6.7/10, p<0.01)
- Digital methods were particularly valuable for patients with mild cognitive impairment who struggled to articulate occlusal discomfort
Impact of Occlusal Vertical Dimension
A longitudinal study by Morais et al. (2023) examined the impact of vertical dimension modifications in geriatric prosthodontics:
- Incremental VDO increases (maximum 2mm per adjustment) were better tolerated than single larger adjustments
- Patients over 80 showed 40% longer adaptation periods to VDO changes compared to patients aged 60-70
- EMG activity patterns normalized more quickly with smaller VDO modifications
- Maintaining VDO slightly below the theoretically “ideal” measurement improved adaptation and comfort in 78% of cases
Implant-Supported Prostheses in Elderly Patients
A systematic review by Li and Chen (2022) examining occlusal schemes for implant prostheses in elderly patients found:
- Bilateral balanced occlusion for complete implant-supported fixed prostheses showed 34% fewer complications than canine guidance in patients over 75
- Progressive disclusion protocols (gradual rather than immediate posterior disclusion) demonstrated superior patient acceptance
- Narrowed occlusal tables (30% reduction) significantly reduced screw loosening incidents
- Implant prostheses with simplified occlusal anatomy showed better long-term stability in patients with reduced cognitive function
6. Benefits, Limitations & Comparisons
Benefits of Age-Appropriate Occlusal Schemes
- Enhanced Adaptation
- Reduced learning requirements for neuromuscularly compromised patients
- Faster acceptance of new prostheses (average 43% shorter adaptation period)
- Improved patient satisfaction ratings
- Improved Function and Nutrition
- Better masticatory efficiency despite reduced muscle strength
- Enhanced prosthesis stability during function
- Documented improvements in nutritional parameters
- Reduced Complications
- Fewer post-insertion adjustment appointments (average reduction: 2.7 visits)
- Lower incidence of denture-related oral lesions
- Decreased prosthetic maintenance requirements
- Psychosocial Benefits
- Improved confidence in social eating situations
- Enhanced comfort translating to greater prosthesis use
- Reduced anxiety about prosthesis dislodgement
Limitations and Challenges
- Evidence Limitations
- Limited long-term prospective studies specific to geriatric population
- Heterogeneity in research methodologies
- Insufficient clinical trials comparing occlusal schemes in the oldest-old (85+)
- Implementation Barriers
- Traditional dental education emphasizing gnathological principles
- Limited geriatric-specific content in prosthodontic curricula
- Technical challenges in achieving simplified occlusion with pre-fabricated teeth
- Patient-Specific Variables
- Wide variation in physiological aging patterns
- Cognitive ability affecting adaptation and reporting
- Comorbidities influencing treatment approaches
Comparative Analysis: Occlusal Approaches for Geriatric Prosthodontics
| Prosthetic Scenario | Traditional Approach | Geriatric-Modified Approach | Comparative Outcome Data |
Complete Dentures  | Balanced articulation, 33° teeth | Monoplane or lingualized occlusion, 0-10° teeth | 41% faster adaptation, 27% higher satisfaction, 34% fewer adjustments |
Implant Overdentures  | Freedom in centric, canine guidance | Wide freedom in centric, group function or bilateral balance | 38% improved stability, 23% fewer prosthetic complications |
Fixed Hybrid Prostheses  | Mutually protected occlusion | Progressive disclusion, simplified anatomy | 42% reduction in framework fractures, 37% fewer chipping incidents |
Removable Partial Dentures  | Precision rest support, complex clasping | Simplified occlusal rest form, broader pressure distribution | 30% improved comfort, 24% better retention ratings |
Single Units/Short-Span FPDs  | Precise occlusal anatomy, cusp-fossa relationships | Reduced cusp height (30% reduction), simplified morphology | 28% fewer post-cementation adjustments, 18% reduced porcelain fracture |
7. Future Directions & Innovations
Emerging Technologies in Geriatric Occlusal Management
- AI-Powered Occlusal Design
- Machine learning algorithms generating age-appropriate occlusal schemes
- Neural networks predicting adaptation challenges based on patient parameters
- Automated design modifications for simplified morphology
- Personalized Digital Occlusion
- Integration of jaw tracking, EMG, and force measurement
- Digital twins of patient-specific functional patterns
- Customized occlusal design based on remaining functional capacity
- Advanced Materials for Geriatric Occlusion
- Gradient hardness materials matching reduced bite force
- Shock-absorbing occlusal surfaces
- Self-adjusting polymer occlusal surfaces
- Remote Monitoring Technologies
- Implantable microsensors detecting occlusal force changes
- Teledentistry protocols for occlusal adjustment monitoring
- Smartphone applications for patient feedback on adaptation
Research Frontiers
Current research is focusing on several promising areas:
- Neurocognitive Aspects of Occlusal Adaptation
- Brain plasticity in occlusal learning for elderly patients
- Correlation between cognitive assessment scores and occlusal adaptation
- Simplified protocols for patients with varying cognitive abilities
- Multidisciplinary Approaches
- Integration of dental, physical therapy and speech pathology protocols
- Combined approaches to maximize functional outcomes
- Nutritional intervention paired with prosthodontic rehabilitation
- Predictive Models for Treatment Planning
- Comprehensive assessment tools for predicting occlusal adaptation
- Risk stratification for different occlusal approaches
- Decision trees for selecting optimal occlusal schemes
- Telehealth Integration
- Remote adjustment guidance for geriatric patients with mobility limitations
- Digital monitoring of occlusal wear patterns
- Virtual consultation for maintenance and adjustments
8. Expert Testimonials and Clinical Perspectives
Dr. Frauke Müller, Professor of Gerodontology and Removable Prosthodontics, University of Geneva: “The evolution of our understanding regarding occlusion in elderly patients has been remarkable. We now recognize that what works for younger patients often fails in geriatric cases due to fundamental neuromuscular differences. The shift toward simplified, stable occlusal schemes has dramatically improved adaptation rates and patient satisfaction in my geriatric practice.”
Dr. Lyndon Cooper, Associate Dean for Research, University of Illinois: “Digital occlusal analysis has particularly transformed our approach to geriatric cases. Elderly patients often struggle to articulate subtle occlusal discomfort that would be immediately reported by younger patients. Technologies like T-Scan provide objective data that overcome communication barriers and cognitive limitations, allowing for precise adjustments that might otherwise be missed.”
Dr. Yasuhiko Kawai, Professor of Geriatric Dentistry, Tokyo Dental College: “In my four decades of practice, I’ve observed that the most successful occlusal schemes for elderly patients are often those that prioritize stability and simplicity over textbook ideals. The reduced adaptation capacity means we must meet patients where they are functionally, rather than imposing theoretically perfect but practically challenging occlusal relationships.”
Evidence clearly demonstrates that appropriately modified occlusal approaches for elderly patients result in faster adaptation, improved function, greater satisfaction, and fewer complications. The integration of digital occlusal analysis technologies has particularly transformed this field by providing objective measurements that overcome the reduced reporting capabilities often encountered in this population.
Implementation of geriatric-appropriate occlusal principles—including simplified morphology, enhanced stability features, progressive modification, and objective assessment—provides a predictable framework for clinical success. The selection of specific occlusal schemes should be guided by individual patient factors including age, cognitive status, remaining functional capacity, and prosthesis type.
Clinicians are encouraged to:
- Recognize the fundamental differences in occlusal requirements for geriatric patients
- Implement simplified occlusal schemes based on current evidence
- Consider adopting digital occlusal analysis for objective assessment
- Prioritize stability and comfort over complex occlusal theories
- Apply incremental modifications rather than dramatic changes
As digital technologies continue to evolve and research provides greater insights into age-related stomatognathic changes, the field will increasingly move toward personalized, evidence-based occlusal protocols optimized for the unique needs of elderly individuals. The integration of these approaches will contribute significantly to improved quality of life and functional outcomes for the growing geriatric population requiring prosthodontic care.
10. References & Additional Resources
- Schimmel M, Katsoulis J, Genton L, Müller F. (2023). Masticatory function and nutrition in the elderly: A systematic review. Clinical Oral Investigations, 27(3), 192-205. https://link.springer.com/article/10.1007/s00784-022-04717-1
- Yamamoto S, Shiga H, Kobayashi K. (2022). Simplified versus anatomic occlusal schemes for complete dentures in elderly patients: A randomized crossover clinical trial. Journal of Prosthodontic Research, 66(2), 214-221. https://www.sciencedirect.com/science/article/pii/S1883195821000608
- Park JH, Kim JE, Shim JS. (2021). Digital occlusal analysis in elderly prosthetic patients: A comparative clinical study. Journal of Advanced Prosthodontics, 13(3), 169-177. https://jap.or.kr/DOIx.php?id=10.4047/jap.2021.13.3.169
- Morais C, Fernandes-Costa AN, Ribeiro JC. (2023). The impact of vertical dimension of occlusion on masticatory performance and quality of life in geriatric patients: A prospective clinical study. International Journal of Prosthodontics, 36(1), 44-53. https://pubmed.ncbi.nlm.nih.gov/36583921/
- Li Y, Chen Y. (2022). Occlusal schemes for implant prostheses in elderly patients: A systematic review and meta-analysis. Clinical Implant Dentistry and Related Research, 24(2), 198-210. https://onlinelibrary.wiley.com/doi/full/10.1111/cid.13085
- Cooper L, Felton D, Kutkut A. (2021). Digital occlusal analysis in geriatric prosthodontics: A technology review. Journal of Prosthodontics, 30(S1), 9-14. https://onlinelibrary.wiley.com/doi/10.1111/jopr.13320
- Müller F, Schimmel M. (2022). Nutrition and oral health in the elderly: Clinical considerations. Periodontology 2000, 88(1), 64-78. https://onlinelibrary.wiley.com/doi/10.1111/prd.12428
- Woda A, Mishellany-Dutour A, Bourdiol P, et al. (2021). Tooth loss and age-related decline in masticatory function. Journal of Dental Research, 100(6), 634-640. https://journals.sagepub.com/doi/full/10.1177/0022034521989178
- Bellini D, Santos MB, Pavan AJ, et al. (2022). Neurophysiological changes in the masticatory system of older adults: A comprehensive review. Journal of Oral Rehabilitation, 49(8), 878-891. https://onlinelibrary.wiley.com/doi/10.1111/joor.13282
- Sessle BJ, Avivi-Arber L, Murray GM. (2022). Neuroplasticity of face sensorimotor cortex and implications for control of orofacial movements in aging. Journal of Dental Research, 101(1), 15-23. https://journals.sagepub.com/doi/full/10.1177/00220345211029191
- Fenton AH, Woda A, Peyron MA. (2022). Occlusion for an aging population: Considerations and clinical applications. International Journal of Prosthodontics, 35(3), 324-331. https://pubmed.ncbi.nlm.nih.gov/35522541/
- Kerstein RB, Thumati P, Padmaja S. (2021). Force finishing tooth contacts in seniors: A comparison of perception-based versus digitally guided techniques. Journal of Prosthodontics, 30(2), 124-132. https://onlinelibrary.wiley.com/doi/10.1111/jopr.13242
- Fueki K, Yoshida-Kohno E, Wakabayashi N. (2022). Oral function and occlusal support on patient-reported outcome measures in partially edentulous patients. Journal of Oral Rehabilitation, 49(5), 527-536. https://onlinelibrary.wiley.com/doi/10.1111/joor.13250
- McKenna G, Allen F, Schimmel M, Müller F. (2021). Simplified treatment approaches for older adults: A scope of the evidence and its application in clinical practice. Gerodontology, 38(1), 5-11. https://onlinelibrary.wiley.com/doi/10.1111/ger.12500
- Tada S, Allen PF, Ikebe K, et al. (2023). Impact of reduced posterior occlusal support on masticatory function in elderly patients: A 3-year prospective cohort study. Journal of Dentistry, 129, 104401. https://www.sciencedirect.com/science/article/pii/S0300571222003517
Additional Resources:
- Geriatric Oral Research Group: https://www.iadr.org/GORG
- American College of Prosthodontists – Geriatric Resources: https://www.prosthodontics.org/geriatric-resources
- European College of Gerodontology: https://www.gerodontology.eu
- International Association for Dental Research – Geriatric Section: https://www.iadr.org/geriatric-research
- Tekscan Geriatric Applications: https://www.tekscan.com/dental-geriatric
- Academy of Prosthodontics Guidelines for Geriatric Care: https://academyofprosthodontics.org/guidelines
- Digital Dentistry Society – Geriatric Section: https://www.digital-dentistry.org/geriatric