Implantology & Guided Surgery Innovations
Keywords: Digital implant planning, guided implant surgery, CBCT for implants, intraoral scanning, dynamic navigation, static guides, 3D-printed surgical guides, digital wax-ups.
Abstract
Modern implantology has embraced fully digital workflows to enhance precision, predictability, and patient outcomes. The integration of CBCT imaging, intraoral scanning, and digital wax-ups allows clinicians to perform highly accurate, minimally invasive implant placements. Additionally, guided surgery techniques have evolved into two main categories: dynamic navigation systems and static 3D-printed surgical guides. This article explores these technological advancements, their clinical applications, and their impact on implant success rates.
Introduction
The evolution of implantology and guided surgery has significantly improved accuracy, surgical efficiency, and patient satisfaction. Traditional freehand implant placement, though widely practiced, is subject to operator-dependent variability. The advent of digital implant planning and guided surgical techniques has minimized these uncertainties by providing precise pre-surgical visualization and real-time guidance.
The shift toward fully digital workflows and navigation-assisted implant placement represents a paradigm change, reducing risks and optimizing prosthetic outcomes.
A. Fully Digital Implant Planning
mplantology has evolved dramatically with the integration of digital workflows, allowing clinicians to achieve unparalleled accuracy, efficiency, and predictability in implant placement. Fully digital implant planning utilizes advanced imaging, computer-assisted treatment planning, and AI-driven simulations to optimize implant positioning before the surgery even begins.
Traditional implant planning methods relied heavily on 2D radiographs, manual measurements, and freehand placement, often leading to variations in outcomes. In contrast, fully digital workflows eliminate guesswork, enhance precision, and improve patient outcomes by incorporating CBCT imaging, intraoral scanning, digital wax-ups, and 3D treatment planning software.
Key Components of Fully Digital Implant Planning
1. CBCT (Cone Beam Computed Tomography) for 3D Bone Analysis
CBCT is the foundation of digital implant planning, providing high-resolution, three-dimensional imaging of the patient’s bone structure, sinus positioning, nerve pathways, and soft tissues. Unlike traditional panoramic X-rays, CBCT scans offer:
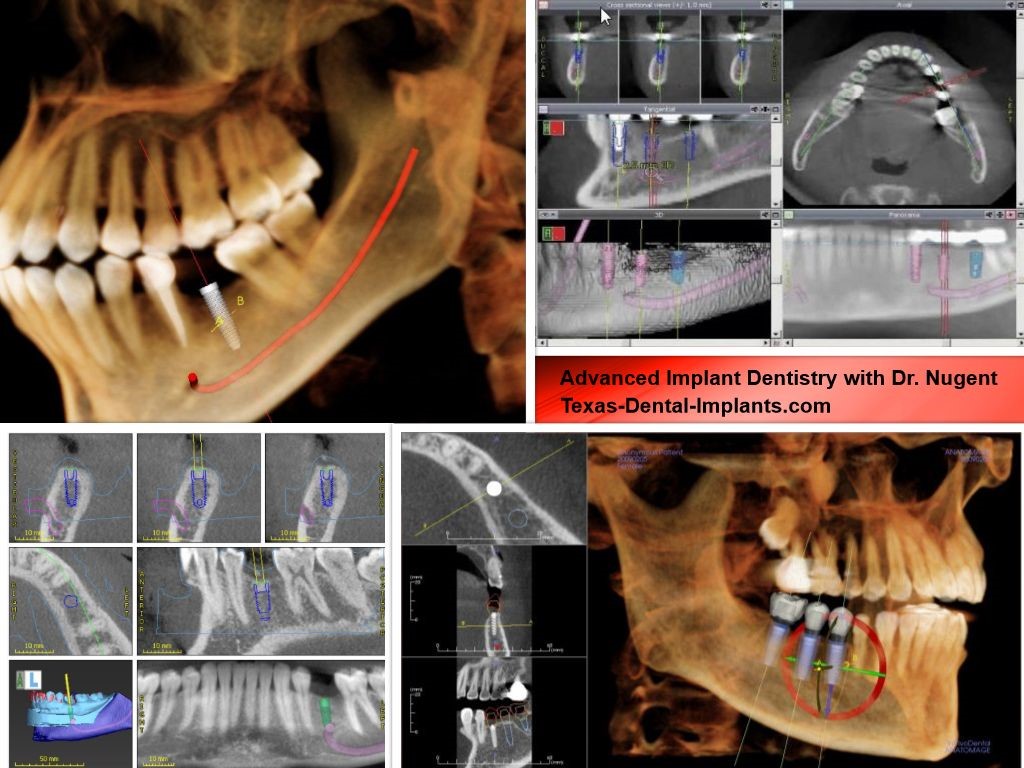
- Accurate bone density mapping, helping clinicians determine whether additional procedures like bone grafting are required.
- Precise anatomical visualization, ensuring implants are placed in an optimal location to avoid nerves and sinus cavities.
- Improved prosthetically driven planning, where implant positioning is determined not just by bone availability but by final restoration requirements.
CBCT imaging is seamlessly integrated into digital planning software, allowing for precise implant trajectory simulation before surgery.
2. Intraoral Scanning: Replacing Traditional Impressions

Intraoral scanners have replaced traditional impression materials, offering a faster, more comfortable, and highly accurate method to capture a patient’s dentition. The benefits of intraoral scanning in digital implant planning include:
✔ Higher accuracy – No distortion compared to conventional impressions.
✔ Immediate data transfer – Digital scans can be uploaded instantly into planning software.
✔ Better patient experience – Eliminates discomfort associated with traditional impression materials.
✔ Enhanced soft tissue mapping – Helps in planning implant emergence profiles and soft tissue contours.
Popular intraoral scanning systems, such as iTero, TRIOS (3Shape), and Medit i700, integrate seamlessly with digital implant software to ensure precision from scanning to surgery.
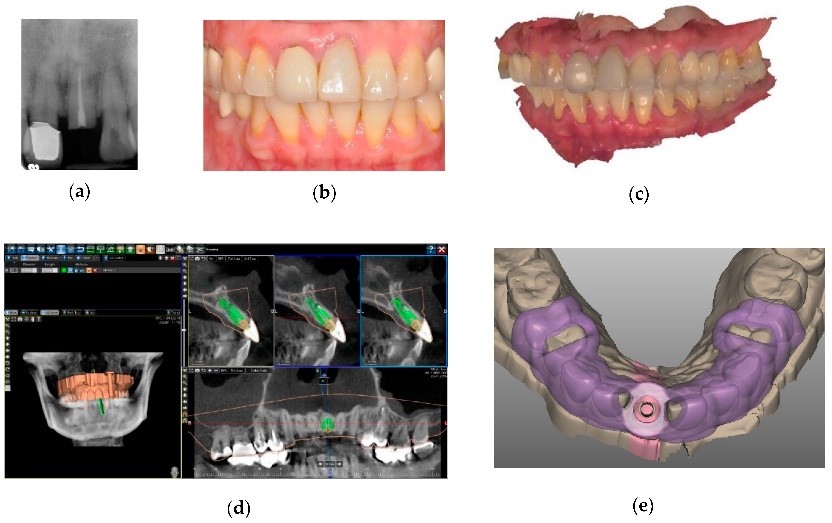
3. Digital Wax-Ups & Prosthetically Driven Planning
In modern implantology, prosthetically driven planning has become a fundamental approach to ensure the long-term success, functionality, and aesthetics of dental implants. Rather than placing implants based solely on bone availability, this method prioritizes the final prosthetic outcome, ensuring implants are positioned to best support the restoration, occlusion, and overall oral function.
A critical component of prosthetically driven implant planning is the use of digital wax-ups—virtual models that allow clinicians to visualize the final restoration before any surgical intervention occurs. These wax-ups, created through computer-aided design (CAD) software, help plan the ideal implant positioning, angulation, and emergence profile, minimizing complications and maximizing patient satisfaction.
1. What Are Digital Wax-Ups?
Digital wax-ups are three-dimensional virtual models of a patient’s proposed final prosthetic restoration created using digital dentistry software. These models mimic the natural anatomy, occlusion, and esthetic contours of the intended dental work, enabling precise preoperative planning.
Traditional vs. Digital Wax-Ups
- Traditional wax-ups involved creating manual wax models on stone casts, which required significant time and effort.
- Digital wax-ups are designed in CAD software, offering greater precision, flexibility, and efficiency.
How Digital Wax-Ups Are Created
- Intraoral scanning captures the patient’s existing dentition, soft tissue, and bite relationship.
- CBCT imaging provides three-dimensional visualization of bone structure and anatomical landmarks.
- The data is imported into CAD software, where the ideal prosthetic design is created digitally.
- The digital model allows for pre-surgical modifications and simulations, ensuring optimal implant positioning and esthetic results.
2. The Importance of Prosthetically Driven Implant Planning
Prosthetically driven implant planning ensures that the final restoration looks natural and functions optimally. Unlike traditional methods that focus primarily on bone availability, this approach prevents misaligned implants that can lead to compromised prosthetic designs and occlusal issues.
Key Considerations in Prosthetically Driven Planning
- Implant Position & Angulation – Aligning the implant to the planned final restoration.
- Occlusal Functionality – Ensuring proper bite alignment and force distribution.
- Aesthetic Integration – Positioning the implant to support a natural smile line.
- Soft Tissue Support – Designing the implant emergence profile to allow for healthy gingival contours.
When implants are placed without proper prosthetic planning, complications such as unnatural crown length, soft tissue recession, and bite misalignment can occur. Digital wax-ups eliminate these risks by allowing clinicians to design and evaluate the final restoration before implant placement.
3. Integration of Digital Wax-Ups with CBCT & Intraoral Scanning
A predictable implant placement requires the seamless integration of CBCT imaging, intraoral scanning, and digital wax-ups.
Step-by-Step Workflow for Digital Implant Planning
- Capture Patient Data
- Intraoral scanners provide a detailed digital impression of the patient’s dentition.
- CBCT scans offer precise bone structure analysis and location of vital structures such as sinuses and nerves.
- Create a Digital Wax-Up
- The prosthetic design is modeled virtually in CAD software.
- The ideal implant position is determined based on the final restoration.
- Simulate the Implant Placement
- Virtual simulations assess occlusion, angulation, and esthetic parameters.
- Fabricate a 3D-Printed Surgical Guide (if required)
- Static guided surgery can be used to ensure precise implant placement based on the digital plan.
This fully digital workflow improves implant accuracy and reduces surgical time and complications.
4. Advantages of Digital Wax-Ups in Implantology
- Predictability and Accuracy – Eliminates guesswork and ensures precise implant placement.
- Enhanced Prosthetic Design – Restorations are planned before surgery, avoiding esthetic or occlusal issues.
- Minimized Risk of Implant Complications – Proper angulation reduces peri-implant stress and soft tissue problems.
- Improved Communication – Allows collaboration between dentists, oral surgeons, and lab technicians.
- Time Efficiency – Digital workflows reduce the need for manual adjustments, expediting treatment timelines.
4. AI-Powered Implant Planning & Virtual Simulations
AI-driven software is revolutionizing implant planning by:
🔹 Automating implant positioning based on ideal bone structure and prosthetic needs.
🔹 Predicting potential complications, such as inadequate bone volume or incorrect angulation.
🔹 Simulating treatment outcomes before surgery, ensuring more predictable results.
🔹 Reducing the need for post-surgical modifications, minimizing patient discomfort and treatment duration.
AI-integrated planning software, such as NobelClinician, SimPlant, and Blue Sky Plan, allows clinicians to visualize implant placement from multiple angles, simulate bite forces, and create highly accurate surgical guides.
Clinical Advantages of Fully Digital Implant Planning
✔ Higher Precision & Accuracy – Eliminates human error associated with manual measurements and freehand placement.
✔ Minimally Invasive Surgery – More precise pre-surgical planning leads to smaller incisions, less trauma, and faster healing times.
✔ Enhanced Communication – Digital workflows allow seamless collaboration between prosthodontists, surgeons, and lab technicians.
✔ More Predictable Outcomes – AI-driven analysis helps optimize treatment, reducing the risk of implant failure.
✔ Shorter Treatment Times – Efficient digital workflows reduce the time required for implant placement and restoration.
B. Dynamic Navigation vs. Static Guided Surgery
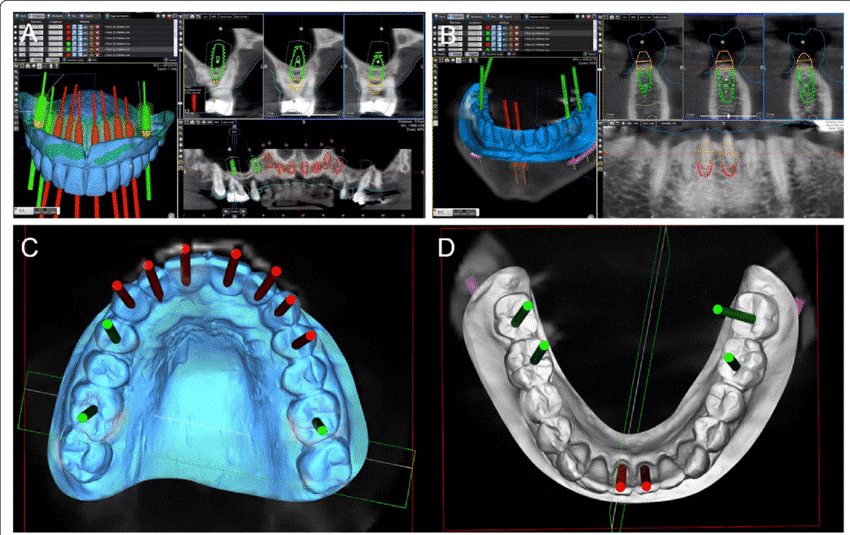
1. Static Guided Surgery: The Role of 3D-Printed Surgical Guides
- Uses pre-planned digital implant placement data to fabricate custom 3D-printed surgical guides.
- Guides assist in precise angulation and depth control, reducing operator error.
- Requires CBCT and intraoral scans, followed by guide fabrication using CAD/CAM technology.
🔹 Advantages:
- High surgical accuracy, especially for multiple implants.
- Cost-effective compared to real-time navigation.
- Shorter surgical time, as the guide ensures rapid drilling execution.
🔹 Limitations:
- Requires additional time for guide fabrication, causing surgical delays.
- No real-time adaptability—if bone quality differs from the plan, modifications cannot be made mid-surgery.
2. Dynamic Navigation Systems: Real-Time Surgical Guidance
- Utilizes motion-tracking cameras and computer-assisted navigation to guide implant drills in real time.
- The system provides live feedback, allowing mid-procedure modifications based on bone density, anatomical variations, or unexpected complications.
- Navigation tools such as X-Guide by X-Nav Technologies and Navident by ClaroNav provide submillimeter accuracy.
🔹 Advantages:
- Real-time adaptability, allowing the clinician to modify implant positioning intraoperatively.
- Eliminates the need for pre-fabricated surgical guides, reducing preoperative delays.
- Enhances freehand precision, especially in challenging anatomical sites.
🔹 Limitations:
- Higher costs due to specialized equipment.
- Requires clinician training, adding to the learning curve.
- Slightly longer chairside time compared to static guides.
3. Comparative Analysis: Dynamic vs. Static Guided Surgery
| Feature | Static Guided Surgery | Dynamic Navigation |
| Preoperative Planning | Required (CBCT & digital guide) | Required (CBCT & software setup) |
| Real-Time Adjustments | No | Yes |
| Accuracy | High | High (submillimeter precision) |
| Cost | Lower | Higher |
| Learning Curve | Minimal | Requires training |
| Surgery Time | Shorter | Slightly longer |
Conclusion
The adoption of fully digital implant planning and guided surgery techniques has significantly enhanced implant placement precision and treatment predictability. The integration of CBCT, intraoral scanning, and digital wax-ups ensures optimized prosthetic outcomes, while navigation-assisted systems further refine surgical execution.
Both static guided surgery and dynamic navigation offer unique advantages, with static guides excelling in cost-effectiveness and simplicity, while dynamic systems provide real-time adaptability and enhanced accuracy. The choice between these technologies depends on case complexity, clinician experience, and financial considerations.
As AI, digital workflows, and real-time guidance technologies continue to evolve, the future of implantology is poised for further innovation, efficiency, and improved patient care.
References & Additional Resources
- Clinical studies on CBCT-guided implant placement and digital workflows.
- Research on AI in implantology and guided surgery precision.
- Manufacturer documentation on dynamic navigation systems and 3D-printed guides.
- Case studies comparing static and dynamic surgical outcomes.

