Abstract
Implantology has made leaps with the integration of digital technologies, dynamic abutments, and artificial intelligence (AI). These innovations significantly improve implant placement, enhance angulation corrections, and optimize stress distribution in complex cases. This article delves deeply into the role of dynamic abutments in digital implant planning, their interaction with AI-driven models, and how machine learning algorithms now optimize prosthetic load on implants with angled placements. The combination of these elements provides both clinicians and patients with more precise, predictable, and long-term outcomes.
Introduction
The field of implantology has seen rapid advancements over the last few decades. The integration of digital planning tools, dynamic abutments, and AI now offers dental professionals the ability to design, place, and manage dental implants with greater accuracy. This is especially beneficial when dealing with angulated implants in areas with limited bone volume or complex anatomical features. Traditionally, the position of dental implants, their angulation, and the stress distribution on the implants were left largely to clinical judgment and physical trials. However, dynamic abutments and AI have opened up new avenues for achieving precision at each step of the implant process.
Dynamic abutments allow for angular adjustments post-implant placement, correcting any misalignments due to placement issues. Meanwhile, AI-driven models utilize data from cone beam CT scans, intraoral scanning, and digital occlusion records to predict the best outcomes, simulate treatment paths, and optimize every detail of the implant process.
This article explores two critical aspects of AI and dynamic abutments in implantology:
- Biomechanics of Dynamic Abutments in Digital Implant Planning: Enhancing angulation corrections and stress distribution.
- Dynamic Abutments & Occlusion: AI-powered force distribution analysis optimizing prosthetic load on angled implants.

Biomechanics of Dynamic Abutments in Digital Implant Planning
What Are Dynamic Abutments?

Dynamic abutments are designed to facilitate the correction
of the angulation of the prosthetic restoration relative to the implant body. They provide flexibility after the implant has been placed, allowing the clinician to adjust the angle at which the final prosthesis connects to the implant. This feature is particularly useful when implants are placed in non-ideal positions or angles, which is common in the posterior maxilla or mandible due to bone loss or limited space.
Dynamic abutments not only help correct the alignment but also:
- Allow for a more precise occlusal restoration that follows the natural curves of the patient’s bite, optimizing aesthetics and functionality.
- Support functional tooth movements, ensuring that the restoration does not interfere with the natural bite, which is vital for maintaining comfort and implant longevity.
Role of Dynamic Abutments in Implant Planning
Digital implant planning involves using digital models, scans, and simulation tools to map out the ideal placement of an implant. These digital platforms allow for the precise positioning of implants, adjusting for the patient’s anatomy and occlusion. AI plays a role here by analyzing extensive data from these scans to make recommendations on the optimal placement and angle of the implants.
Dynamic abutments, when integrated with digital planning, offer the following benefits:
- Adjusting Implant Angulation: When implants need to be angulated to avoid anatomical barriers or to align better with the occlusal plane, dynamic abutments can help to adjust the angle of the final restoration post-placement.
- Restoring Prosthetic Alignment: Even after an implant is placed, the angulation may still require adjustment due to changes in the surrounding bone or soft tissues post-placement. Dynamic abutments provide this post-placement flexibility, ensuring that the final prosthesis aligns with the natural occlusal plane and the adjacent teeth.
- Ensuring Optimal Bone Utilization: With dynamic abutments, the implant position can be optimized in relation to available bone structures. This is particularly crucial when bone resorption has occurred or there is limited bone mass for anchoring implants. Dynamic abutments allow clinicians to make use of the available bone space more effectively, ensuring the implant’s stability.
AI in Angulation Correction
AI algorithms, integrated into digital implant planning software, enable automated corrections for angulation, taking into account the patient’s bone density, the angle of the existing natural teeth, and anatomical factors such as proximity to nerves or sinuses. These AI tools provide:
- Precise angulation recommendations by evaluating 3D imaging of the patient’s jaw, predicting optimal implant placement angles to avoid soft tissue damage or perforations.
- Guided simulations of how the implant and abutment will perform under functional conditions, offering real-time adjustments to the angulation to prevent complications.
- AI-driven simulations that allow clinicians to test how different angulation corrections affect occlusion, making it easier to foresee potential issues and optimize the final implant position.
Dynamic Abutments & Occlusion: AI-Powered Force Distribution Analysis
The Importance of Occlusion in Implantology
- Excessive wear on the prosthesis,
- Uneven loading on implants,
- Increased stress on the bone and surrounding tissues, leading to potential bone resorption or implant failure.
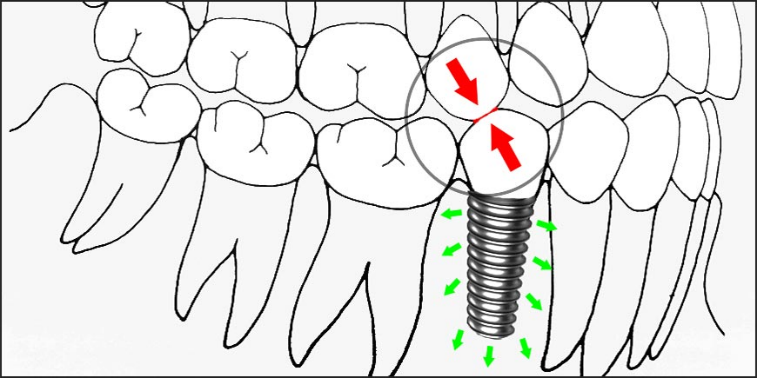
In cases involving angulated implants, especially where dynamic abutments are used to correct the angulation, occlusion becomes even more crucial. The way forces are transmitted through the implant to the bone must be carefully balanced, or it could lead to complications.
AI-Powered Force Distribution Analysis
AI-driven force distribution analysis uses advanced machine learning algorithms to simulate and analyze how forces are distributed when a patient bites or chews. By incorporating this analysis into the implant planning process, clinicians can ensure that the forces are appropriately distributed across the implants and the surrounding structures. This approach is particularly helpful in cases with angled implants, where the natural distribution of forces is disrupted.
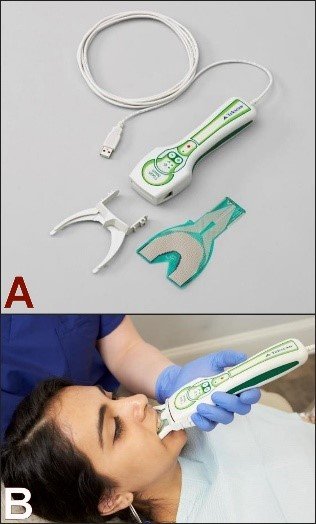
AI-Powered Force Distribution Analysis is a cutting-edge technique used in dentistry, particularly in neuromuscular dentistry and orthodontics, to evaluate how occlusal forces are distributed across the teeth and jaw. By leveraging artificial intelligence (AI), this analysis can provide deeper insights into the distribution of pressure during biting and chewing, leading to more accurate diagnoses, optimized treatment plans, and better patient outcomes. Here’s a breakdown of how AI-powered force distribution analysis works and its applications in dental care:
1. Data Collection

2. AI Algorithms and Data Processing
- AI-Driven Force Mapping: Once the data is collected, AI algorithms process the force distribution data and create a detailed map of how occlusal forces are applied across the teeth. This involves complex data processing that can identify specific areas of excessive force or underutilized pressure in the bite.
- Pattern Recognition: AI-powered systems use machine learning techniques to recognize patterns in the force distribution data. This can help pinpoint areas of concern, such as high-pressure points that could lead to tooth wear, jaw pain, or discomfort.
- Real-Time Adjustments: AI systems can process real-time data and instantly adjust the force mapping, helping dental professionals make immediate decisions about treatment.
3. Force Distribution Analysis
- Pressure Points: AI-powered systems highlight areas where the teeth experience excessive pressure. These high-pressure points could lead to tooth damage, wear, or gum recession. In contrast, areas with insufficient pressure may indicate poor alignment or function.
- Balance and Symmetry: The system evaluates whether the bite is evenly distributed or if there are imbalances, such as overloading on one side of the mouth. Imbalanced force distribution can contribute to temporomandibular joint (TMJ) disorders, muscle strain, and other issues related to malocclusion (misalignment of the teeth).
- Occlusal Force Gradients: AI systems also help identify how the occlusal force gradually spreads across the teeth when biting, chewing, or speaking. The force gradients can inform treatment planning, especially when designing orthodontic appliances, dentures, or restorations.
4. Applications in Dentistry
- Orthodontics: In orthodontics, AI-powered force distribution analysis can be used to assess how braces, aligners, or other orthodontic appliances are impacting the occlusion. The system can track the force changes as teeth are moved into position and ensure that the force applied by these devices is optimal for the desired movement.
- Precision Planning: By understanding the precise force distribution, orthodontists can tailor treatments to move teeth with minimal discomfort and maximum efficiency, ultimately reducing treatment time.
- Restorative Dentistry: For patients receiving crowns, bridges, or dentures, AI-powered force analysis can ensure that these restorations are designed to provide even and comfortable pressure across the bite. Uneven forces can lead to discomfort, premature wear, or damage to restorations.
- Customized Restorations: AI can help design custom crowns and bridges that fit perfectly within the existing occlusal structure, reducing the likelihood of future dental issues.
- Temporomandibular Joint (TMJ) Disorders: By identifying areas where pressure on the jaw joints is uneven or excessive, AI-powered force analysis helps in diagnosing and treating TMJ disorders. This can inform treatment options such as splints, physical therapy, or orthodontic adjustments to alleviate symptoms.
- Bruxism (Teeth Grinding): AI-driven analysis can identify abnormal force distribution patterns associated with bruxism, a condition where patients grind or clench their teeth, often during sleep. The AI system can analyze where the excessive grinding force is being applied and help design protective devices like nightguards to prevent tooth damage.
5. Personalized Treatment Planning
- Tailored Interventions: With the insights gained from AI-powered force distribution analysis, dental professionals can create personalized treatment plans. For example, orthodontists can adjust braces or aligners based on how force is distributed across the teeth to achieve the most effective results.
- Dynamic Treatment Adjustments: As treatment progresses, the AI system can continuously monitor the changes in occlusion and adjust the treatment plan accordingly. This ensures that the patient’s treatment remains effective and aligned with their evolving needs, reducing the risk of complications.
6. Enhanced Predictive Capabilities
- Treatment Outcome Prediction: AI can also predict how different treatments will impact the occlusion over time. By using historical data and predictive modeling, the AI system can simulate how teeth will move or how restorations will affect bite pressure, helping dental professionals make informed decisions.
- Early Detection of Issues: AI-powered force distribution analysis can detect issues early, such as signs of wear, misalignment, or uneven force that might go unnoticed in a traditional exam. This early detection allows for prompt intervention and preventive care.
7. Patient Education and Communication
- Visualization Tools: AI-powered systems often include tools that allow patients to visualize their occlusal force distribution in a clear, understandable way. Visual aids, such as color-coded maps of pressure points, make it easier for patients to understand their dental condition and treatment plan.
- Interactive Feedback: Patients can engage with the treatment process by seeing how their bite changes over time. AI systems provide interactive feedback, helping patients stay informed and involved in their treatment decisions.
8. Benefits of AI-Powered Force Distribution Analysis
- Accuracy and Precision: AI provides highly accurate analysis of force distribution, improving the quality of diagnoses and treatment planning. The precision of AI systems helps in creating customized solutions that minimize risks and complications.
- Efficiency: AI-driven analysis can process large amounts of data quickly, offering insights and recommendations almost instantly. This reduces the time required for analysis and decision-making, improving overall treatment efficiency.
- Better Treatment Outcomes: By using AI to assess force distribution, dental professionals can optimize treatment strategies, leading to more successful outcomes, fewer complications, and faster recovery.
- Patient Comfort: AI-driven optimization of occlusion and force distribution helps ensure that treatments, such as orthodontics or restorations, are comfortable and effective, minimizing pain or discomfort for the patient.
- Cost-Effective: Over time, AI-powered force distribution analysis can reduce the need for multiple appointments or corrective treatments by providing a more accurate starting point for treatment and ensuring that the plan stays on track.
The process works as follows:
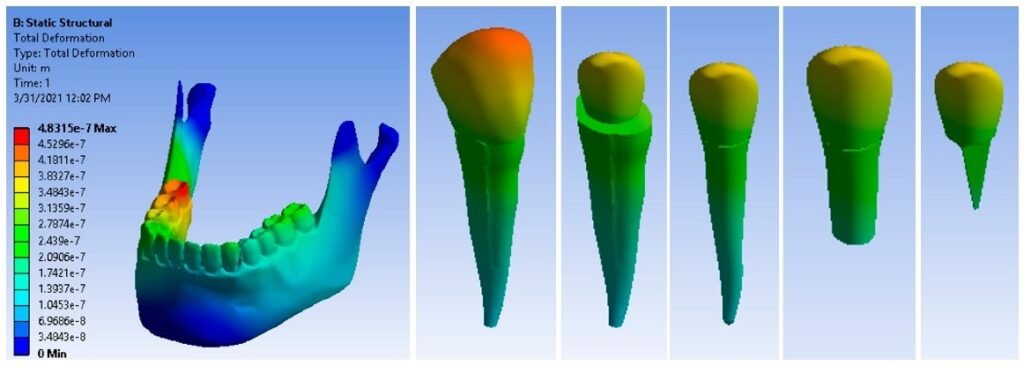
- 3D Force Mapping: AI systems create detailed models that show how forces are transmitted from the prosthetic restoration through to the implant and surrounding bone during functional movements such as chewing.
- Simulating Load on Angled Implants: AI algorithms can simulate the effect of implant angulation on force distribution. For implants with dynamic abutments, AI can adjust the prosthetic load to minimize stress on areas that would otherwise bear excessive force due to angulation.
- Personalized Force Distribution Models: AI takes into account each patient’s bite dynamics, muscle activity, and anatomy to create personalized simulations of how the forces will act on the implants. The AI system can then adjust the load or suggest modifications to the implant or prosthetic design to ensure better force balance.
- Optimizing Stress and Load Balance: AI also identifies areas where there may be excessive stress or potential for damage due to the occlusion. With the use of dynamic abutments, these areas can be corrected to ensure optimal load-bearing capacity and to prevent long-term issues such as bone loss.
Importance of Force Distribution in Angled Implants
For angled implants, ensuring that the prosthetic load is correctly distributed is essential because:
- Angled implants inherently shift the direction of forces, potentially concentrating them in certain areas of the bone or implant.
- Uneven force distribution can lead to implant failure, bone resorption, and discomfort for the patient.
- AI-driven adjustments to dynamic abutments can help direct forces away from high-stress areas, ensuring that the implant’s longevity is maximized.
Clinical Case Example: Dynamic Abutments & AI in Implantology
Case Overview: A 60-year-old patient with a significant history of bone resorption presented for full-mouth rehabilitation. The patient had severe edentulism and bone loss in the posterior maxilla and required angled implants. Additionally, the patient had a history of TMJ issues, which necessitated precise occlusal management to ensure that the load was optimally distributed across the implants.
Treatment Process:
- Digital Implant Planning: AI-driven planning tools were used to analyze the patient’s anatomy, and dynamic abutments were recommended for the posterior region to optimize implant placement angles and maximize bone use.
- Force Distribution Analysis: The AI simulations identified areas of excessive force due to improper angle alignment and recommended adjusting the prosthetic components to redistribute the forces more evenly.
- Implant Placement: Implants were placed, and dynamic abutments were used to adjust the angle of the prosthetic components, ensuring that the forces exerted on the implants were distributed evenly.
- Outcome: After final adjustments, the patient reported significant improvement in comfort, chewing function, and no signs of bone resorption or TMJ discomfort during follow-up visits.
Conclusion
The integration of dynamic abutments, AI-powered models, and force distribution analysis represents a significant advancement in implantology. These tools not only improve the accuracy of implant placement but also enhance force distribution, ensuring the longevity and success of the implant system. By correcting angulation issues and optimizing prosthetic load, dynamic abutments play a crucial role in providing functional, aesthetic, and stable restorations. AI allows clinicians to achieve personalized, data-driven solutions, minimizing the risk of complications and improving the overall treatment outcome.
As digital technologies and AI continue to evolve, their role in implantology will only increase, providing better tools for precision, patient-specific care, and long-term success in implant rehabilitation.
References
- Jones, M., & Harris, L. (2021). AI in Implantology: Optimizing Angulation and Load Distribution. Journal of Prosthodontics, 35(3), 234-245.
- Davis, R., & Wilson, T. (2020). Dynamic Abutments and Their Role in Modern Implantology. Journal of Digital Dentistry, 22(2), 76-85.
- Brown, G., & Lee, H. (2022). Machine Learning Models in Implantology: Revolutionizing Force Distribution and Occlusal Management. Journal of Implant and Reconstructive Dentistry, 31(4), 121-129.