Introduction: The Evolution of Smile Design
Digital Smile Design (DSD) emerged as a revolutionary methodology in the early 2000s, pioneered by Brazilian dentist Dr. Christian Coachman. What began as a simple concept of using digital tools to enhance treatment planning has evolved into a comprehensive philosophy that fundamentally changes how aesthetic dentistry is conceptualized, planned, and executed. Today, DSD represents not merely a technological advancement but a paradigm shift in how dental professionals approach smile enhancement.
The essence of Digital Smile Design lies in its systematic integration of facial analysis, patient-specific desires, functional requirements, and technological precision. This holistic approach recognizes that a truly successful smile enhancement must consider the smile not as an isolated entity but as an integral component of facial aesthetics and personal expression.

Foundational Principles of Digital Smile Design
The Facial-Driven Approach
Unlike traditional dentistry which often begins with tooth preparation, DSD starts with comprehensive facial analysis. This facial-driven approach acknowledges that teeth exist within the larger context of the face and should harmonize with facial features and expressions.
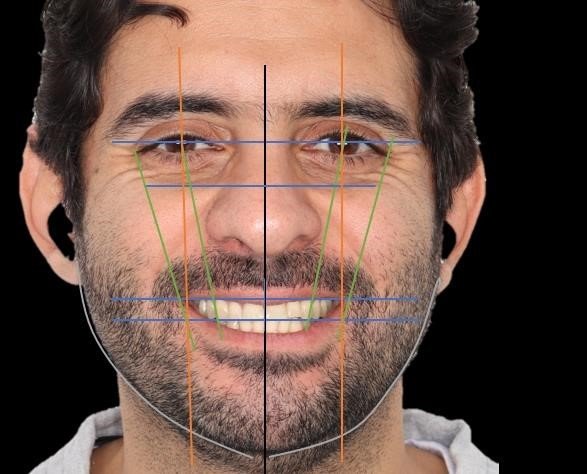
- The bipupillary line (horizontal line connecting the pupils)
- The facial midline
- The commissural line (connecting the corners of the mouth)
- The incisal plane
- The gingival heights and architecture
These references provide objective parameters that guide the design process, ensuring that the final result exists in harmony with the patient’s unique facial characteristics rather than conforming to generic standards of beauty.
Emotional Dentistry Concept
A core philosophical element of DSD is what Coachman terms “emotional dentistry”—the recognition that smile design must account for the emotional impact of the smile on both the patient and observers. This involves careful consideration of:
- Tooth display during various expressions: Not just the full smile, but also the resting position, speech, and laughter
- Personality-driven design: Creating smiles that reflect the patient’s character and self-image
- Age-appropriate aesthetics: Respecting the natural changes in dental appearance throughout life stages
- Cultural considerations: Acknowledging that aesthetic ideals vary across different cultures and communities
From 2D to 4D Analysis
Modern DSD has evolved from simple two-dimensional planning to a four-dimensional approach:
- Static 2D analysis: The evaluation of facial and dental proportions in photographs
- Static 3D analysis: The assessment of volume, depth, and spatial relationships
- Dynamic analysis: Observing how dental structures interact with facial movements during speech and expression
- Temporal dimension: Considering how the smile design will age and function over time
This multi-dimensional approach enables practitioners to create smiles that not only look beautiful in photographs but function harmoniously in daily life and maintain their aesthetic value over time.
The Comprehensive DSD Protocol
Initial Documentation Phase
The foundation of successful DSD implementation begins with meticulous documentation that captures all relevant patient information:
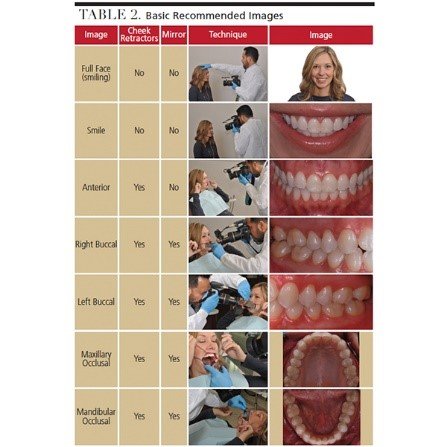
A standardized photographic series is essential, typically including:
- Full face photographs (resting, full smile, profile, and oblique views)
- Close-up smile images (with and without retractors)
- Occlusal views (maxillary and mandibular arches)
- 12 o’clock view (from above the patient’s head looking down at the smile)
These photographs must be taken with proper camera settings, consistent lighting, and correct patient positioning to ensure accurate analysis. DSLR cameras with macro lenses and ring flashes have become the standard equipment for this purpose, though some clinicians now utilize specialized dental photography systems with standardized settings.
Video Documentation
Dynamic video recording captures crucial information that static photographs cannot, including:
- Natural speech patterns
- Transition between expressions
- Lip mobility and dynamics
- Dynamic tooth display during various expressions
- Patient’s description of their aesthetic concerns in their own words
The videographic assessment typically includes recordings of the patient pronouncing specific phonemes (especially “F,” “V,” and “S” sounds) to evaluate anterior tooth display during speech, as well as spontaneous and posed smiles to assess differences between social and emotional expressions.
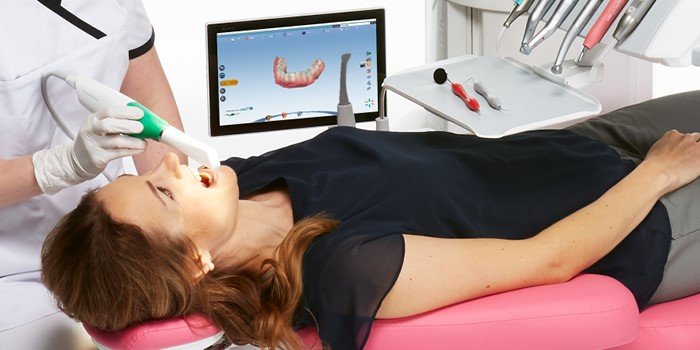
Digital Impressions and Scanning
Contemporary DSD protocols increasingly incorporate digital impressions rather than traditional physical impressions. Intraoral scanners generate highly accurate three-dimensional models of the patient’s dentition that can be seamlessly integrated with facial scans and photographs. Advanced scanning systems now capture not just tooth morphology but also soft tissue architecture and even color data, providing comprehensive information for the planning phase.
Analysis and Design Phase
With comprehensive documentation complete, the systematic analysis begins:
Facial Analysis
The facial analysis establishes key reference lines and planes:
- Horizontal references: Beyond the bipupillary line, additional horizontal references include the interpupillary line, commissural line, and the natural horizon line. Cross-referencing these helps identify facial asymmetries that might affect smile design.
- Vertical references: The facial midline serves as the primary vertical reference, but it’s crucial to distinguish between the geometric midline (dividing the face into equal halves) and the aesthetic midline (the perceived center of the face), which may differ due to natural asymmetries.
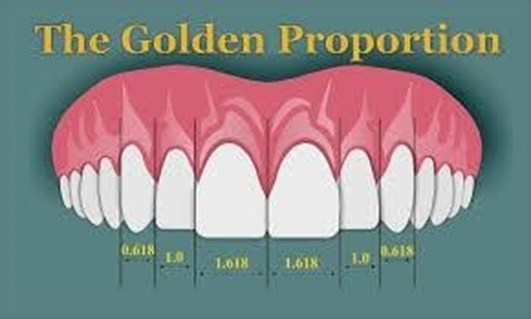
- Golden proportions assessment: While not applied rigidly, the facial analysis often includes evaluation of classical proportional relationships, such as the rule of thirds (dividing the face vertically) and the rule of fifths (dividing the face horizontally).
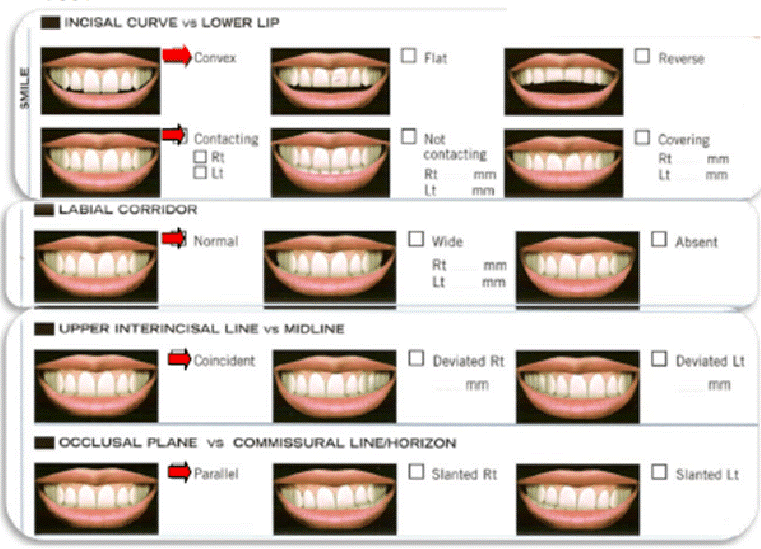
Dento-labial Analysis
This examines the relationship between the teeth and lips:
- Smile line: Categorizing the smile as high (revealing significant gingival display), medium, or low (showing limited tooth structure).
- Buccal corridor: Evaluating the negative space visible between the buccal surfaces of the posterior teeth and the corners of the mouth during smiling.
- Lip support: Analyzing how the teeth support the lips in both resting and dynamic states.
Dento-gingival Analysis
The relationship between teeth and gingival tissues significantly impacts smile aesthetics:
- Gingival zenith positions: Identifying the most apical point of the gingival margin for each tooth, with particular attention to the lateral incisors (typically positioned 0.5-1mm below the central incisors and canines).
- Gingival architecture: Assessing the shape, texture, and color of the gingival tissues, as well as the presence of papillae between teeth.
- Biological width evaluation: Ensuring that proposed restorations respect the natural attachment apparatus of the periodontium to prevent inflammation or recession.
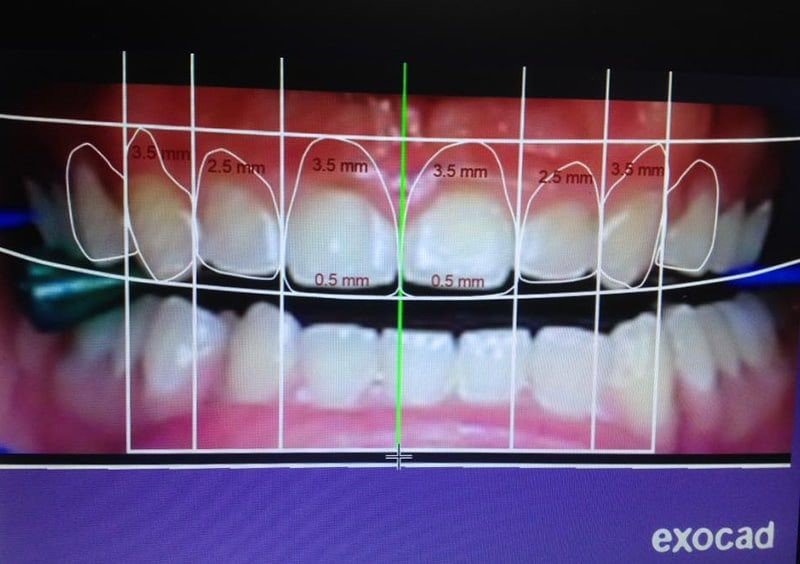
Dental Analysis

The detailed examination of the teeth themselves focuses on:
- Tooth proportions: Evaluating width-to-length ratios, typically aiming for central incisors with a 75-80% width-to-length ratio.
- Tooth axes: Assessing the inclination of teeth relative to vertical reference lines, with progressive inclination typically increasing from central incisors to canines.
- Incisal edge position: Determining the optimal position of anterior incisal edges in relation to the upper lip, phonetics, and occlusal function.
- Surface morphology: Analyzing the existing tooth surfaces for characterization elements such as lobes, grooves, and translucency patterns that might be incorporated into the new design.
Digital Waxup Creation
Using specialized DSD software platforms (such as DSD Planning Center, Smile Designer Pro, or NemoDSD), the clinician creates a digital waxup—a virtual model of the proposed smile design:
- Digital tooth arrangement: Individual teeth are digitally designed with consideration for proper proportions, alignments, and relationship to reference lines.
- Surface characterization: Details such as developmental grooves, incisal characterization, and surface texture are incorporated for natural appearance.
- Material selection simulation: The software may simulate different restorative materials to predict their optical behavior in various lighting conditions.
Modern DSD software platforms offer increasingly sophisticated tools including:
- Automated smile library suggestions based on facial morphology
- Virtual articulation to assess functional movements
- Integration with CAD/CAM systems for direct restoration fabrication
- Artificial intelligence-assisted design recommendations
Patient Presentation and Co-design
A distinguishing feature of DSD is the emphasis on patient involvement in the design process:
- Digital mockup presentation: The proposed design is presented to the patient through before-and-after images, showing how the new smile will look in the context of their face.
- Virtual reality visualization: Some advanced practices now offer VR headsets that allow patients to “wear” their proposed smile and view it from different angles.
- Co-design session: Rather than simply presenting a finished design, DSD practitioners engage patients in a co-design process, making real-time adjustments based on patient feedback.
- Emotional assessment: The presentation phase includes evaluation of the patient’s emotional response to the proposed design, which often reveals subtle preferences that weren’t articulated during initial consultations.
Prototype Phase: The Mock-up
Once the digital design is approved, it’s transferred to a physical prototype:
- 3D printing of design models: The digital waxup is 3D printed to create a physical model.
- Silicone index creation: A silicone matrix is fabricated from the printed model to transfer the design to the patient’s mouth.
- Intraoral mock-up: Using bis-acryl composite material, a temporary version of the smile design is created directly on the patient’s existing teeth without any preparation.
This crucial step allows the patient to “test drive” their new smile, evaluating:
- Aesthetics in different lighting conditions and environments
- Speech function
- Comfort
- Social reaction
- Emotional response
The mock-up phase may last from hours to several weeks, depending on the complexity of the case and the extent of patient adaptation required. During this period, refinements can be made based on patient feedback before finalizing the treatment plan.
Treatment Planning and Sequencing
With the design validated through the mock-up, a comprehensive treatment plan is developed:
- Interdisciplinary planning: The approved design serves as a blueprint for all team members, which may include:
- Orthodontist for preliminary tooth alignment
- Periodontist for gingival architecture modification
- Oral surgeon for skeletal or implant considerations
- Prosthodontist for final restorations
- Digital treatment sequencing: A step-by-step sequence is established, often visualized through digital progression models showing each treatment phase.
- Material selection: Specific restorative materials are selected based on aesthetic requirements, functional demands, and biological considerations.
- Laboratory communication: Detailed specifications are provided to the dental laboratory, including the approved digital design files, material selections, and shade information.
Guided Clinical Implementation
The approved design guides all clinical procedures:
- Minimally invasive preparation: Tooth preparation is performed with direct reference to the approved design, often using preparation guides derived from the digital waxup to ensure minimal tooth reduction.
- Immediate temporization: Provisional restorations closely matching the approved design are placed immediately after preparation.
- Guided tissue management: For cases requiring gingival recontouring, surgical guides derived from the digital design ensure precise tissue modification.
- Final restoration integration: The definitive restorations are evaluated against the original design parameters before final cementation.
Advanced Technologies Enhancing Digital Smile Design
Facial Scanning Technologies
Facial scanning has evolved significantly from simple 2D photography:
- Stereophotogrammetry: Systems like 3dMD capture high-resolution 3D facial images in milliseconds, eliminating motion artifacts and providing true 3D representations of soft tissue.
- Smartphone-based scanning: Emerging applications utilize smartphone cameras with specialized algorithms to generate detailed 3D facial models accessible to practices without expensive dedicated scanning equipment.

These technologies enable the integration of precise soft tissue information with dental data, creating comprehensive virtual patient models.
Intraoral Scanning Advancements
The evolution of intraoral scanners has significantly enhanced the accuracy and efficiency of digital impressions:
- High-speed scanners: Modern scanners capture full-arch scans in under a minute with sub-100 micron accuracy.
- Color and texture mapping: Advanced scanners record not just morphology but also color information, allowing for more realistic digital models.
- AI-enhanced scanning: Artificial intelligence algorithms automatically identify margin lines, detect defects, and even suggest optimal preparation modifications.
CAD/CAM Integration
Computer-aided design and manufacturing systems have become seamlessly integrated with DSD workflows:
- Direct design transfer: Approved smile designs can be directly imported into CAD software for restoration design without information loss.
- In-office fabrication: For suitable cases, designs can be milled or printed in a single visit using chairside CAD/CAM units.
- Digital articulation: Virtual articulators simulate jaw movements to ensure functional harmony of the proposed design.
- Material-specific optimization: CAD software now incorporates material-specific parameters to optimize the performance of different ceramics, composites, or hybrid materials.
Augmented Reality Applications
Augmented reality represents the newest frontier in DSD technology:
- Real-time smile simulation: AR applications overlay the proposed smile design on the patient’s face in real-time, allowing them to see how the new smile looks while speaking and expressing emotions.
- Interactive design adjustment: Some AR systems permit real-time modification of the design while the patient observes the changes.
- Social context visualization: Advanced applications can place the virtual smile in different social settings or lighting conditions to provide a more comprehensive preview.
Clinical Applications and Case Selection
Comprehensive Aesthetic Rehabilitation
DSD is particularly valuable for cases requiring full-mouth rehabilitation, where the establishment of a clear aesthetic blueprint guides functional reconstruction. These cases often involve:
- Severely worn dentition
- Multiple missing teeth
- Significant occlusal discrepancies
- Combined fixed and removable prosthetics
The DSD approach ensures that functional rehabilitation achieves optimal aesthetics rather than addressing function and aesthetics as separate concerns.
Minimally Invasive Veneer Cases
For patients seeking aesthetic enhancement with minimal biological cost, DSD enables precisely planned veneer preparations that respect tooth structure while achieving the desired outcome. The mock-up phase is particularly valuable in these cases, as it:
- Guides precisely how much tooth reduction is necessary (if any)
- Allows evaluation of the proposed contours before irreversible preparation
- Serves as a preparation guide during the procedure

Implant-Supported Restorations
The integration of DSD with implant planning software creates powerful synergies:
- Prosthetically driven implant placement: The approved smile design determines optimal implant positions to support the desired restoration.
- Guided surgery integration: DSD-approved tooth positions can inform the creation of surgical guides for precise implant placement.
- Immediate provisionalization: The digital design facilitates the fabrication of immediate provisional restorations that establish optimal soft tissue contours from the outset.
Orthodontic-Restorative Cases
For cases requiring tooth movement before restorative treatment, DSD provides:
- Clear outcome visualization: The final aesthetic goal is established before orthodontic treatment begins.
- Optimal tooth positioning: Orthodontic movement is planned specifically to achieve ideal position for subsequent restorations.
- Interdisciplinary communication: The shared digital design ensures that orthodontist and restorative dentist work toward a common vision.
Implementation Considerations and Challenges
Learning Curve and Skill Development
Mastering DSD requires developing several interconnected skill sets:
- Technical proficiency: Becoming comfortable with the various software platforms and digital tools involved in DSD implementation.
- Photography and documentation: Learning proper photographic techniques and standardized documentation protocols.
- Aesthetic analysis: Developing the ability to systematically analyze facial and dental aesthetics beyond subjective impression.
- Interdisciplinary coordination: Building skills in communicating design parameters across specialties.
Most clinicians find that implementing DSD requires a gradual adoption approach, starting with simpler cases and progressively tackling more complex situations as confidence grows.
Infrastructure Requirements
Practices implementing DSD need to consider several infrastructure elements:
- Hardware requirements:
- High-quality camera equipment
- Powerful computer systems for processing large image files
- Calibrated monitors for accurate color representation
- Optional: 3D scanners, intraoral scanners, and 3D printers
- Software ecosystem:
- DSD planning software
- Image editing software
- 3D modeling applications
- Practice management integration
- Team capabilities:
- Staff training for documentation procedures
- Case presentation protocols
- Digital workflow management
Financial Considerations
The implementation of DSD requires careful financial planning:
- Initial investment: The acquisition of necessary equipment and software represents a significant upfront cost.
- Learning period efficiency impact: During the initial learning phase, DSD cases may require more time, potentially affecting practice productivity.
- Fee structure adaptation: Practices must develop appropriate fee structures that reflect the additional value provided through DSD while remaining competitive.
- Return on investment timeline: Most practices find that DSD implementation shows positive ROI within 12-24 months through improved case acceptance, reduced remakes, and increased referrals.
Future Directions in Digital Smile Design
Artificial Intelligence Integration
AI is rapidly transforming DSD in several ways:
- Automated analysis: AI algorithms can now identify facial reference points, suggest proportionally ideal tooth arrangements, and even predict patient preferences based on psychological profiles.
- Treatment outcome prediction: Machine learning models are being developed to predict how soft tissues will respond to proposed changes, enhancing the accuracy of the virtual preview.
- Personalized aesthetics: Rather than applying universal beauty standards, AI systems are beginning to recognize individual and cultural variations in aesthetic preference.
Biometric Design Parameters
Moving beyond geometric analysis, emerging approaches incorporate functional and biometric parameters:
- Muscle activity integration: EMG (electromyography) data from facial muscles during expression can be integrated into the design process to ensure harmony with the patient’s natural muscle patterns.
- Masticatory efficiency analysis: Digital occlusal analysis provides data on how proposed designs will function during mastication.
- Phonetic optimization: Acoustic analysis of speech can guide anterior tooth positioning for optimal phonetics.
Materials and Manufacturing Evolution
Advancements in materials science continue to expand DSD possibilities:
- Gradient materials: New ceramics and composites with gradually changing properties can better mimic the complex optical behavior of natural teeth.
- Additive manufacturing: Direct 3D printing of definitive restorations is becoming viable for an increasing range of materials.
- Bioactive materials: Restorative materials that interact positively with biological tissues are being incorporated into digital workflows.
Conclusion: The Transformative Impact of Digital Smile Design
The evolution of DSD continues to accelerate, with each technological advancement bringing new capabilities that enhance both the process and outcomes of smile enhancement. For contemporary dental professionals, mastering DSD represents not merely an adoption of new technology but an embrace of a more comprehensive philosophy that places the patient’s unique facial identity at the center of aesthetic treatment.
As we look to the future, the continued integration of artificial intelligence, biometric analysis, and advanced materials promises to further refine this approach, making truly personalized smile design accessible to more patients while achieving ever more natural and harmonious results. In this ongoing evolution, the fundamental principle of DSD remains constant: creating smiles that enhance not just dental appearance but the overall facial harmony and emotional well-being of each individual patient.