Keywords: digital implant planning, surgical guides, digital dentistry, implant positioning, guided surgery, Exoplan, CBCT, intraoral scanning
Abstract
This comprehensive guide explores the transformative impact of digital planning and custom surgical guides in modern implant dentistry. By leveraging advanced imaging technologies like CBCT and intraoral scanning, practitioners can now achieve unprecedented precision in implant placement. The article outlines the technical specifications for optimal surgical guide design, including critical measurements for implant positioning, sleeve parameters, and anatomical considerations. Through detailed explanations of workflow processes—from data acquisition to guide fabrication—dental professionals will gain practical insights for implementing guided surgery protocols in their practices. This technology-driven approach not only enhances surgical predictability and safety but also improves prosthetic outcomes and patient satisfaction. For clinicians looking to elevate their implant practice through digital workflows, this article provides the essential knowledge and technical parameters required for successful implementation.
Introduction & Background
The integration of digital technologies into implant dentistry has revolutionized treatment planning and surgical execution. Traditional freehand implant placement relied heavily on the clinician’s experience and spatial perception, often leading to variability in outcomes. Today, the combination of 3D imaging, computer-aided design, and guided surgery has created a paradigm shift toward more predictable, precise, and prosthetically-driven implant positioning.
Surgical guides represent the critical link between virtual planning and clinical reality. These patient-specific devices, fabricated based on digital treatment plans, enable surgeons to transfer the exact position, angulation, and depth of planned implants from the computer screen to the patient’s mouth. This transition from digital to clinical environment eliminates much of the guesswork traditionally associated with implant surgery.
Recent advancements in guide design software, such as Exoplan, have further refined this process by allowing meticulous customization of guide parameters based on individual patient anatomy, implant system specifications, and prosthetic requirements. As digital dentistry continues to evolve, understanding the technical aspects of surgical guide fabrication and implementation has become essential for clinicians seeking to optimize their implant protocols.
Main Body Sections
A. Clinical/Technical Overview: Custom Surgical Guides in Digital Implant Planning
Types of Surgical Guides
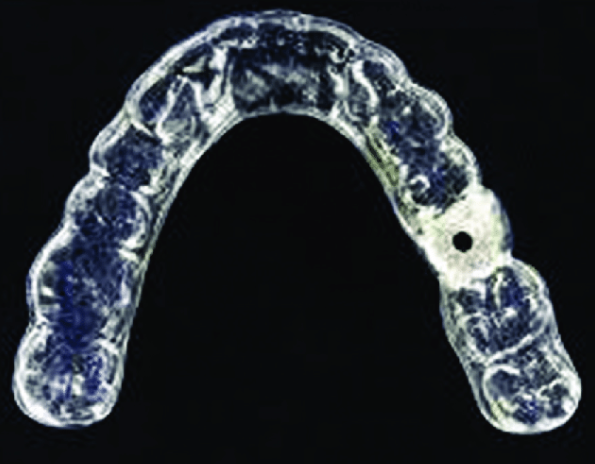
Custom surgical guides translate virtual implant planning into precise surgical procedures through physical templates that direct drill positioning. These guides can be categorized based on their support mechanism:
- Tooth-supported guides

- Utilized when sufficient natural teeth remain to provide stable support
- Offer excellent stability and precision due to the unique surface anatomy of teeth
- Require fewer fixation pins, reducing patient discomfort
- Most commonly used in partially edentulous cases
- Bone-supported guides

- Applied in cases with significant tooth loss where bone exposure is necessary
- Require raising a flap for proper seating on the bony ridge
- Particularly useful in immediate implant placement following extractions
- May require additional fixation pins for stability
- Mucosa-supported guides
- Designed for fully edentulous patients with sufficient soft tissue coverage
- Allow for flapless surgery, reducing post-operative discomfort
- Often incorporate fixation pins to prevent movement during surgery
- May require additional stabilization techniques in cases with mobile mucosa
Technology Integration in Guide Design
The fabrication of surgical guides relies on the integration of multiple digital technologies:
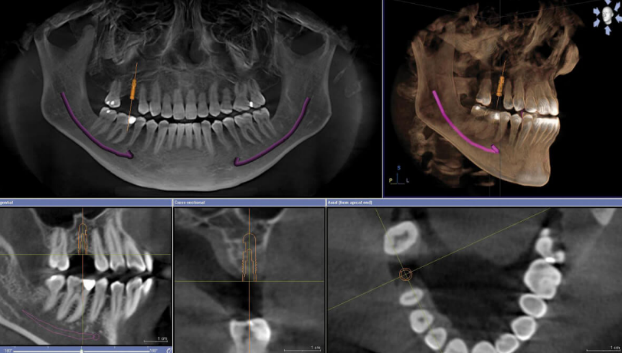
- CBCT (Cone Beam Computed Tomography): Provides 3D visualization of bone volume, density, and vital anatomical structures
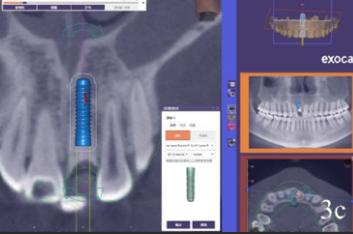
- Intraoral scanning: Captures accurate surface data of teeth and soft tissues for precise guide adaptation
- Planning software (e.g., Exoplan): Allows virtual positioning of implants and design of the surgical guide
- 3D printing/milling: Transforms the digital design into a physical guide with high accuracy
B. Digital Workflow & Technical Specifications
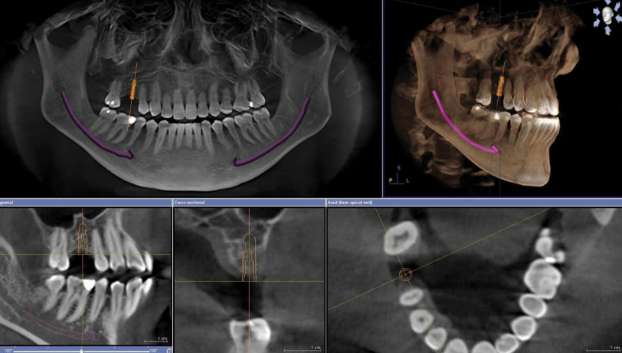
Data Acquisition and Processing
The foundation of accurate surgical guide fabrication lies in proper data acquisition:
- CBCT scan specifications:
- Minimum resolution: 0.3mm voxel size for clear visualization of bone details
- Full arch scans are recommended for comprehensive planning
- Patient positioning must avoid movement artifacts
- Intraoral scan requirements:
- Accuracy within 50 microns for optimal fit of the resulting guide
- Complete capture of adjacent teeth and soft tissues
- Proper scan strategy to minimize distortion
- Data alignment:
- Precise registration of CBCT and intraoral scan data
- Verification of alignment accuracy through anatomical landmarks
- Software-based correction of minor discrepancies
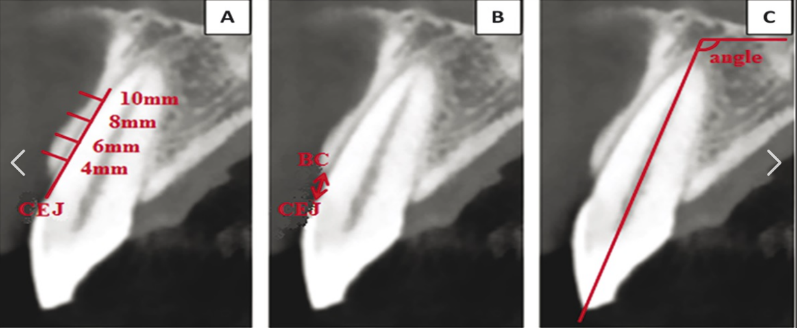
Anatomical Consideration and Boundary Definition
Proper identification and respect for anatomical boundaries are crucial for safe implant placement:
- Mandibular nerve mapping:
- Clear visualization of the inferior alveolar nerve canal
- Maintenance of a minimum 2mm safety distance from the nerve
- Consideration of anatomical variations in nerve position
- Maxillary sinus evaluation:
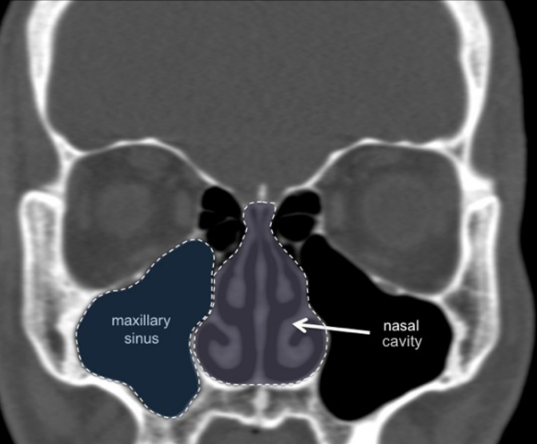
- Assessment of sinus floor morphology
- Maintenance of at least 1mm clearance unless performing a sinus lift
- Consideration of septa and other anatomical variations
- Buccal/Lingual bone assessment:
- Verification of minimum 1mm thickness on both aspects
- Special attention to the esthetic zone, requiring 2mm buccal plate thickness
- Prevention of cortical plate perforation
C. Optimal Implant Positioning Parameters
The long-term success of implant treatment depends on proper three-dimensional positioning:
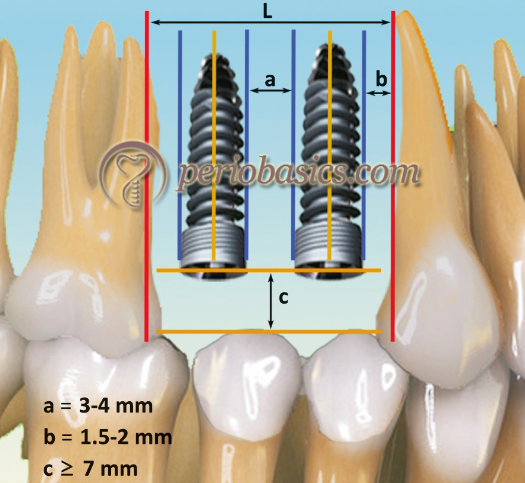
- Mesiodistal positioning:
- Maintain 3mm minimum distance between implants to preserve interproximal bone
- Keep at least 1.5mm from adjacent natural teeth to protect the periodontal ligament
- Center implants within the available space for optimal prosthetic emergence
- Buccolingual positioning:
- Position implant with sufficient bone (minimum 1mm) on both buccal and lingual aspects
- In the esthetic zone, ensure 2mm buccal bone thickness to prevent recession
- Consider the emergence profile requirements for the final restoration
- Apico-coronal positioning:
- Place bone-level implants 2-3mm subcrestally in the esthetic zone
- Adjust depth based on implant system recommendations
- Consider soft tissue thickness for proper emergence profile development
- Implant angulation:
- Maintain angulation within 0-15 degrees of ideal axis to minimize off-axis forces
- Align implant with prosthetic requirements for screw-retained restorations
- Avoid extreme angulations that necessitate custom abutments
D. Surgical Guide Design Specifications

The effectiveness of a surgical guide depends on its design parameters:
- Guide extension and support:
- Tooth-supported guides should cover at least 3-4 stable teeth
- Mucosa-supported guides require 2-3mm tissue contact area for pressure distribution
- Bone-supported guides need a secure fit with a 2mm border around osteotomy sites
- Sleeve parameters and adjustments:

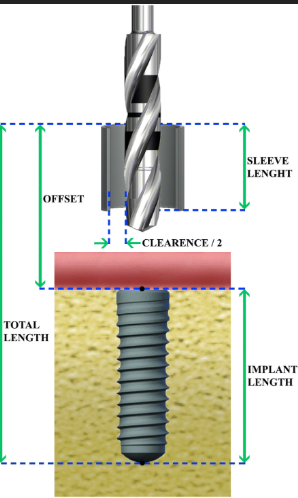

- Inner Diameter (ID): Typically 2.0-5.0mm based on drill system compatibility
- Outer Diameter (OD): Usually 4.5-6.0mm for adequate guide strength
- Height: Between 5-10mm depending on available vertical space
- Offset: 0-3mm to control drill depth relative to implant position
- Additional design considerations:
- Incorporation of ventilation holes (3-4mm diameter) to prevent vacuum effects
- Minimum 1mm clearance from gingival margins to prevent tissue impingement
- Adequate thickness for structural integrity during surgery
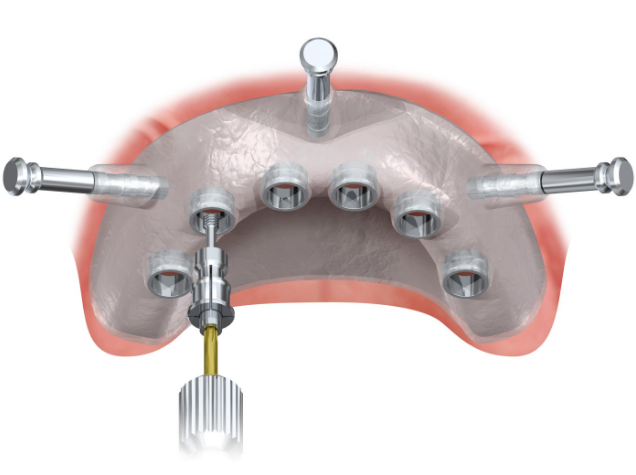
E. Case Study: Full-Arch Rehabilitation Using Digital Planning and Surgical Guides
Patient Presentation
A 62-year-old male patient presented with failing dentition in both arches, seeking a fixed solution for improved function and esthetics. Comprehensive examination revealed generalized periodontal compromise with multiple non-restorable teeth, necessitating full-arch rehabilitation.
Digital Planning Process
- Data acquisition:
- High-resolution CBCT (0.25mm voxel size) captured bone anatomy
- Intraoral scanning documented existing dentition and soft tissue contours
- Facial scanning incorporated for esthetic planning
- Treatment planning:
- Virtual extraction of non-restorable teeth
- Strategic positioning of six implants per arch following “All-on-X” protocol
- Verification of adequate bone volume and identification of anatomical limitations
- Surgical guide design:
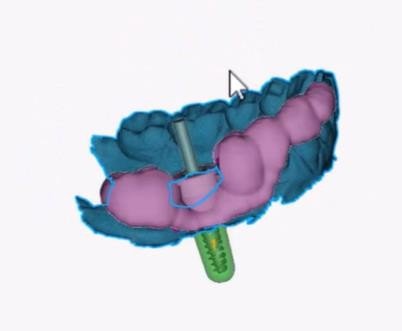
- Tooth-supported guide for immediate guidance following extractions
- Sleeve positioning optimized for surgical access
- Integration of fixation pins for additional stability
Surgical Execution
The surgical guide enabled precise placement of all implants according to the predetermined positions. Immediate loading was possible due to the high primary stability achieved through accurate osteotomy preparation. The patient received provisional restorations the same day, with final prostheses delivered after three months of healing.
Outcome Analysis
Post-operative CBCT confirmed accurate implant positioning with a mean deviation of less than 0.3mm from the planned positions. The patient reported minimal discomfort during and after the procedure. One-year follow-up demonstrated stable osseointegration of all implants and excellent prosthetic function.
F. Product & Technology Comparison
Leading Guided Surgery Systems
| System | Compatible Software | Sleeve System | Accuracy (Published) | Unique Features | Approximate Cost |
Straumann® Guided Surgery  | coDiagnostiX, Exoplan | Fixed-height sleeves | ±0.5mm | Fully guided implant insertion | $$$$ |
Nobel Biocare® NobelGuide 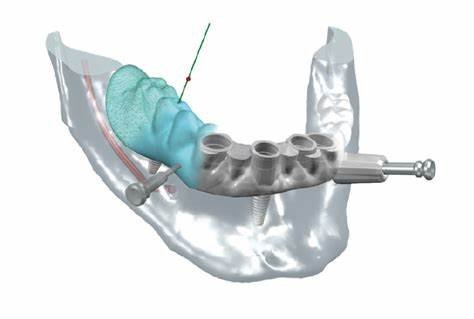 | DTX Studio, Exoplan | Variable-height sleeves | ±0.4mm | Template-based approach | $$$$ |
Zimmer Biomet® Navigator  | RealGUIDE, Exoplan | Universal sleeves | ±0.5mm | Simplified drill protocol | $$$ |
Dentsply Sirona® Simplant 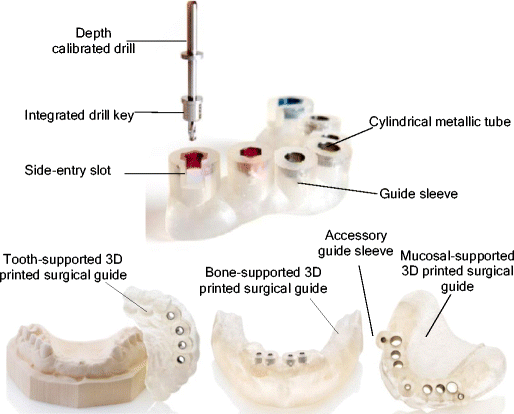 | Simplant, Exoplan | Dedicated sleeve library | ±0.6mm | Comprehensive implant library | $$$$ |
Guide Fabrication Technologies
| Method | Material | Accuracy | Production Time | Cost | Considerations |
3D Printing (SLA/DLP) 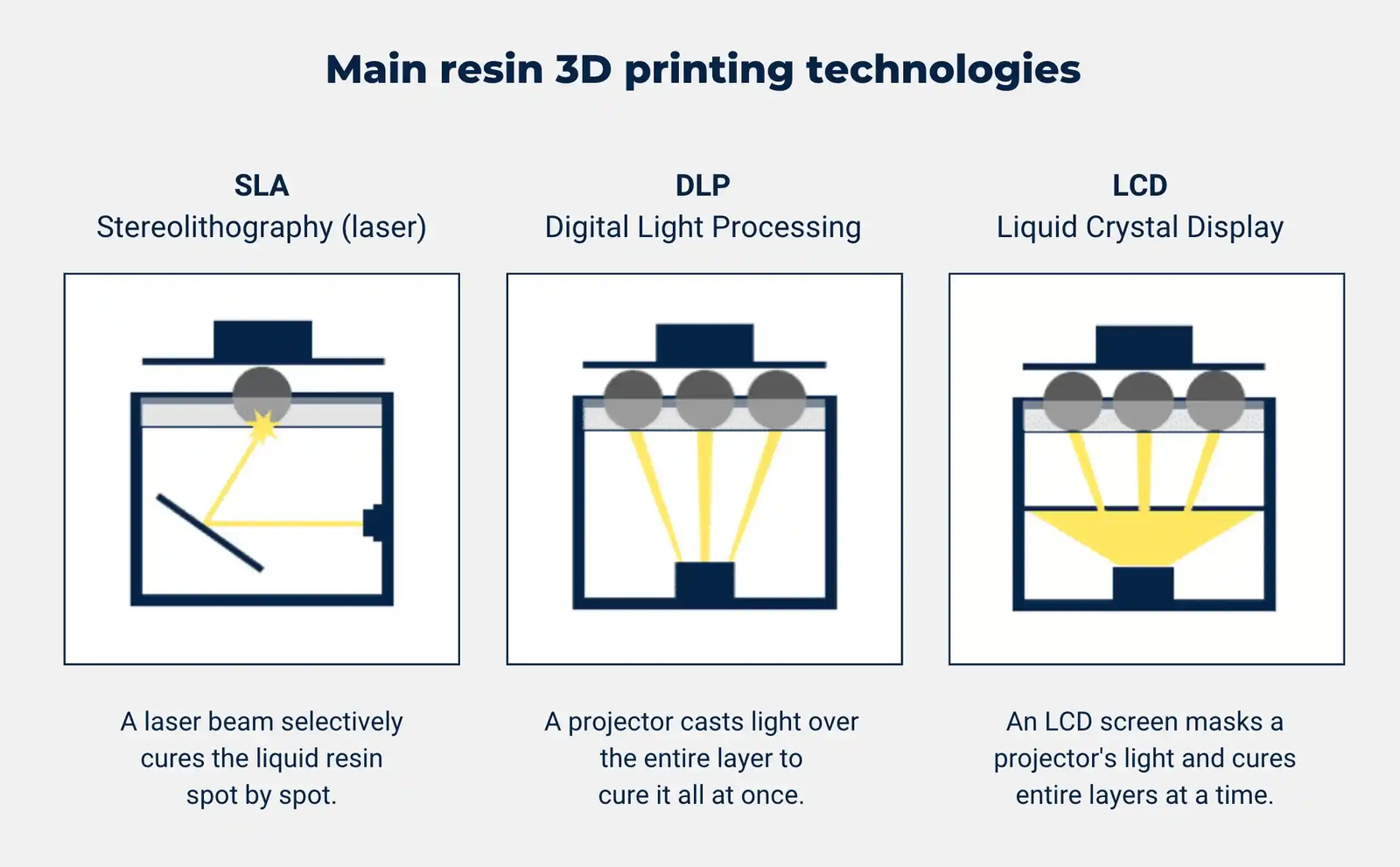 | Biocompatible resin (Class I) | ±50-100 microns | 1-3 hours | $ | Requires post-processing |
| Milling | PMMA blocks | ±30-80 microns | 2-4 hours | $$ | Limited design flexibility |
| Thermoforming | Various polymers | ±100-200 microns | 1-2 hours | $ | Limited precision |
G. Benefits, Limitations & Comparisons
Advantages of Guided Surgery
- Enhanced precision:
- Reduction in placement deviation compared to freehand techniques
- More predictable prosthetic outcomes
- Reduced risk of anatomical complications
- Improved efficiency:
- Shorter surgical time (up to 50% reduction in complex cases)
- Possibility for flapless procedures with faster healing
- Reduced chair time for adjustments
- Better treatment predictability:
- Prosthetically-driven implant positioning
- Facilitation of immediate loading protocols
- Enhanced communication with patients and dental laboratory
Limitations and Challenges
- Technical considerations:
- Learning curve for digital planning software
- Potential for registration errors between CBCT and intraoral scans
- Guide fabrication accuracy limitations
- Clinical limitations:
- Reduced tactile feedback during surgery
- Limited access in patients with restricted mouth opening
- Need for adequate bone volume assessment
- Financial aspects:
- Initial investment in software and equipment
- Per-case costs for guide fabrication
- Additional planning time
Comparison with Traditional Freehand Approach
| Aspect | Guided Surgery | Freehand Approach |
| Precision | High (±0.5mm deviation) | Variable (±2mm deviation) |
| Planning time | Longer (1-2 hours) | Shorter (15-30 minutes) |
| Surgical time | Shorter for complex cases | Longer for complex cases |
| Learning curve | Moderate for software | Steep for surgical skills |
| Cost | Higher initial investment | Lower initial investment |
| Complication rate | Lower (2-5%) | Higher (5-15%) |
H. Future Directions & Innovations
The field of guided implant surgery continues to evolve rapidly with emerging technologies:
- Dynamic navigation systems:
- Real-time tracking of drill position
- Elimination of physical guide fabrication
- Integration with augmented reality displays
- AI-assisted planning:
- Automated detection of anatomical structures
- Suggestion of optimal implant positions based on large datasets
- Prediction of esthetic outcomes
- Robotics in implant surgery:
- Robot-assisted implant placement with haptic feedback
- Integration with real-time monitoring of bone density
- Enhanced precision beyond human capabilities
- Advanced manufacturing techniques:
- Multi-material printing for improved guide properties
- Incorporation of patient-specific antimicrobial agents
- Biodegradable guide materials
References & Additional Resources
- D’haese J, Van De Velde T, Komiyama A, Hultin M, De Bruyn H. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clin Implant Dent Relat Res. 2012;14(3):321-335. doi:10.1111/j.1708-8208.2010.00275.x
- Tahmaseb A, Wismeijer D, Coucke W, Derksen W. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2014;29 Suppl:25-42. doi:10.11607/jomi.2014suppl.g1.2
- Vercruyssen M, Laleman I, Jacobs R, Quirynen M. Computer-supported implant planning and guided surgery: a narrative review. Clin Oral Implants Res. 2015;26 Suppl 11:69-76. doi:10.1111/clr.12638
- Shen P, Zhao J, Fan L, et al. Accuracy evaluation of computer-designed surgical guide template in oral implantology. J Craniomaxillofac Surg. 2015;43(10):2189-2194. doi:10.1016/j.jcms.2015.10.022
- Raico Gallardo YN, da Silva-Olivio IRT, Mukai E, Morimoto S, Sesma N, Cordaro L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28(5):602-612. doi:10.1111/clr.12841
- Exocad GmbH. “Exoplan User Manual – Digital Planning for Implant Dentistry.” https://exocad.com/
- American Academy of Implant Dentistry. “Digital Workflows in Implant Dentistry: Guidelines for Practitioners.” https://www.aaid.com/
- International Team for Implantology (ITI). “SAC Classification in Implant Dentistry.” https://www.iti.org/
Professional Organizations and Resources
- Academy of Osseointegration: https://osseo.org/
- International Congress of Oral Implantologists: https://www.icoi.org/
- Digital Dentistry Society: https://digital-dentistry.org/
- American Academy of Implant Dentistry: https://www.aaid.com/