Computational Biomechanics & Digital Dentistry: Advancing Prosthodontics and Implantology with Finite Element Analysis and Patient-Specific Modeling
Introduction
This article explores the integration of computational biomechanics with digital dentistry, focusing on the application of Finite Element Analysis (FEA) and patient-specific biomechanical modeling. By leveraging digital workflows and advanced AI simulations, these tools are revolutionizing the fields of prosthodontics and implantology. Through real-time biomechanical simulations, dental practitioners can predict stress distribution, optimize implant placement, and improve prosthesis longevity. The utilization of CT/CBCT data further enhances accuracy, while AI-driven simulations offer personalized solutions for occlusal load distribution, ensuring more successful restorative and orthodontic outcomes.
In recent years, computational biomechanics and digital dentistry have brought significant advancements to dental practices, particularly in prosthodontics and implantology. By combining computational models with real patient data, dental professionals can enhance the precision of restorations, optimize implant placement, and extend the lifespan of prostheses. This article delves into how Finite Element Analysis (FEA) and patient-specific biomechanical modeling are reshaping these fields, improving both patient outcomes and procedural efficiency.
Clinical Overview
Computational biomechanics in dental applications primarily involves simulating physical interactions within the body using computational tools. Digital dentistry, enhanced by the use of Finite Element Analysis (FEA), offers a scientific approach to model complex mechanical behavior in dental restorations and implantology.
Finite Element Analysis (FEA) in Prosthodontics & Implantology
Finite Element Analysis (FEA) in prosthodontics and implantology is a computational technique used to simulate and analyze the mechanical behavior of dental materials, restorations, and implant structures under various conditions. It plays a crucial role in optimizing the design, placement, and function of dental prostheses and implants, helping clinicians achieve more predictable and reliable outcomes.
Applications of FEA in Prosthodontics and Implantology:
Finite Element Analysis (FEA) is a powerful computational tool used extensively in prosthodontics and implantology to simulate the behavior of dental materials and structures under various conditions. Here are some key applications of FEA in these fields, sourced from different studies:
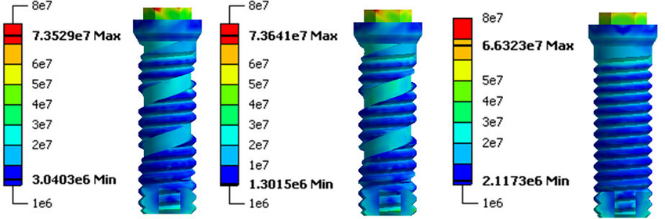
1. Implant Design and Optimization
FEA plays a crucial role in the design and optimization of dental implants. By simulating the mechanical behavior of implants in different bone types, it allows for the refinement of implant geometry, material selection, and surface features to enhance implant stability and longevity.
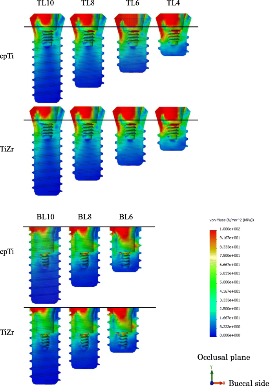
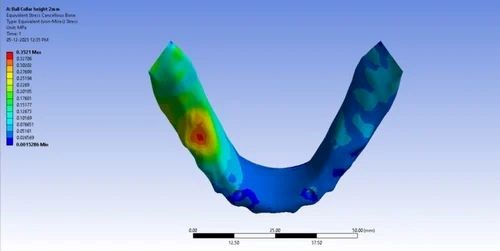
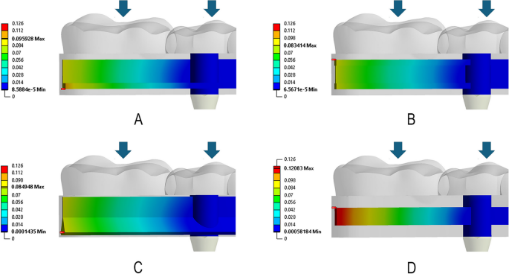
2. Stress Distribution in Implant Systems
One of the most significant contributions of FEA in implantology is its ability to predict and visualize the stress distribution around implants. This is vital to understand how the forces are transmitted from the prosthesis to the underlying bone, which can help prevent bone resorption or failure of the implant system.
3. Prosthesis Design
FEA is employed to design dental prostheses, such as crowns, bridges, and dentures. It helps evaluate the strength and durability of these prostheses under masticatory forces and identify potential failure points.
4. Assessment of Bone-Implant Interface
The bone-implant interface is critical in implantology, as it affects the stability and integration of the implant. FEA can predict how different bone densities and implant surface characteristics influence the bone-implant interface.
- Source: Hagiwara et al., 2009 used FEA to analyze the bone-implant interface and suggested that FEA can predict potential failure modes, such as implant loosening or bone resorption.
5. Simulating Surgical Procedures
FEA can be used to simulate surgical procedures, helping in the planning of dental implant placement. By simulating the cutting and drilling process, FEA can identify the best approach to minimize stress and damage to the surrounding bone.
6. Material Selection
The choice of material for both implants and prostheses is critical for the success of dental treatments. FEA helps simulate the performance of different materials (e.g., titanium, zirconia, and ceramics) under various stress and load conditions to determine the most suitable material for specific clinical applications.
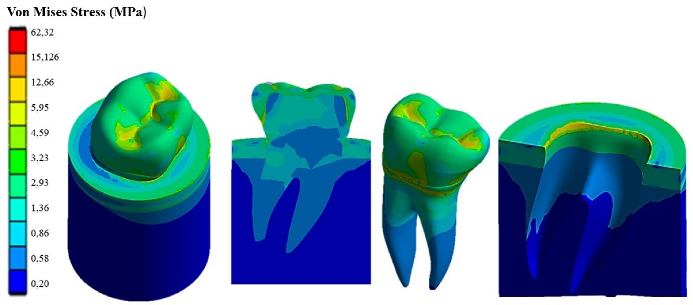
7. Evaluation of Occlusal Forces
Occlusal forces during mastication are dynamic and can affect the longevity of dental implants and prostheses. FEA can simulate these forces, helping to design implants and prostheses that are more resistant to wear and failure.
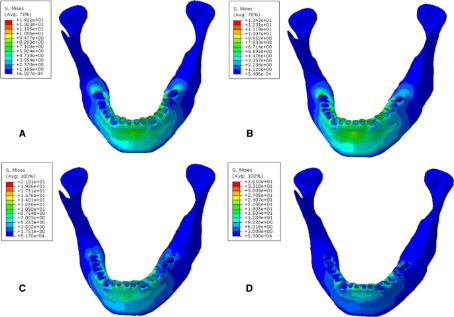
8. Bone Remodeling Prediction
FEA can simulate bone remodeling around implants, predicting how bone will adapt to the presence of an implant over time. This is particularly useful for evaluating long-term implant success and preventing issues like bone loss.
9. Customization of Implants for Individual Patients
FEA allows for the customization of implant systems based on the unique anatomy of a patient’s bone structure. This personalized approach helps in ensuring better outcomes, particularly in cases of challenging bone conditions or anatomical irregularities.
10. Fatigue and Durability Testing
Dental implants and prostheses must withstand repeated loading during normal functions like chewing. FEA is used to simulate long-term fatigue and durability testing, helping predict the lifespan of implants and prostheses.
Challenges and Limitations:
· Modeling Complexity Finite Element Analysis requires the creation of highly detailed models that accurately represent the structures being studied. In prosthodontics and implantology, creating models that capture the full complexity of bone, soft tissue, and implant interactions can be extremely challenging. Any oversimplification can lead to inaccurate results, potentially compromising the design and outcome of treatments.
· Material Properties Accurately modeling the material properties of dental materials and bone is crucial for reliable results. However, the variability in material properties (e.g., bone density and implant surface coatings) across different individuals makes it difficult to create universally accurate simulations. The assumptions made about these materials, such as uniformity or ideal conditions, may not always reflect real-world variability.
· Load and Stress Simulations Real-world forces acting on implants and prostheses are dynamic and multifactorial, involving chewing, grinding, and other movements. Simulating these forces using FEA can be challenging due to the unpredictability of how loads vary across different situations and patient behaviors. Often, static or simplified loading conditions are used, which may not reflect the full complexity of occlusal forces.
· Bone-Implant Interface Variability The interface between the implant and bone is critical for the success of dental implants, and its modeling in FEA can be problematic. The interaction between these two materials is influenced by various factors like bone quality, implant surface texture, and healing processes. Accurately representing these interactions in a finite element model is difficult, and errors in simulation can lead to misguided implant designs or treatment plans.
· Patient-Specific Variability While FEA has the potential to create patient-specific simulations, obtaining accurate and detailed data for individual patients (such as CT scans or MRI) is often resource-intensive. Additionally, slight anatomical variations in bone structure can lead to significant differences in implant behavior, making it hard to create universally applicable models for all patients.
· Time-Consuming Process Building accurate FEA models, conducting simulations, and analyzing results can be time-consuming, especially for complex systems. This process may require advanced software, powerful computing resources, and considerable expertise, which can limit its accessibility in clinical settings.
· Over-Reliance on Simulation FEA is a valuable tool, but it is based on certain assumptions and approximations that may not fully account for all real-world factors. Relying solely on simulation results without considering clinical evidence and patient-specific factors can lead to suboptimal treatment plans. It’s essential to balance FEA insights with clinical judgment and experience.
· Software and Hardware Limitations The accuracy of FEA results heavily depends on the capabilities of the software and hardware used. Some FEA software may have limitations in terms of the complexity of models it can handle or the precision of the results it can provide. Similarly, hardware limitations, such as computational power, can restrict the complexity of the simulations that can be run, reducing the accuracy of the outcomes.
· Cost and Accessibility Advanced FEA tools and the required computational resources can be expensive, which may limit access to these technologies, particularly in smaller dental practices or regions with fewer resources. The initial investment in software, hardware, and training can be a barrier for some professionals, despite the long-term benefits FEA may offer.
· Lack of Standardization FEA methods in prosthodontics and implantology are still evolving, and there is no universal standard for how FEA should be applied or interpreted in dental applications. Variations in software, modeling techniques, and assumptions can lead to different results for similar cases, creating challenges in comparison and validation across studies and clinical practices.
Case Studies
Case Study 1: Use of FEA in Dental Implant Design
A dental clinic utilizes FEA simulations to evaluate the stress distribution around implants placed in the upper jaw. Through the virtual models, they can test different implant shapes and positions to determine which design minimizes the risk of bone resorption and implant failure.
Case Study 2: Enhancing Occlusal Load Distribution in Restorative Dentistry
An orthodontic practice adopts AI-driven biomechanical models to simulate occlusal load distribution for patients undergoing restorative treatments. By adjusting the placement of dental restorations, the practice optimizes load transfer, which reduces wear on the teeth and enhances treatment outcomes.
Product Reviews
- FEA Software for Dental Professionals: Software platforms designed for FEA simulations are increasingly becoming a staple in dental practices. These tools allow practitioners to input patient-specific anatomical data and generate biomechanical models to assess different treatment approaches.
- Patient-Specific Biomechanical Models: Integrating CT/CBCT data with digital workflows creates highly detailed and personalized biomechanical models. These models offer precise information on how forces will interact with the patient’s unique anatomy, leading to more effective treatment planning.
Research & Benefits/Limitations
Research Findings:
- FEA in Prosthodontics: Research shows that FEA can accurately predict the performance of different dental materials under varying conditions. Studies confirm that the optimized placement of crowns, bridges, and implants based on FEA models leads to longer-lasting restorations and fewer complications.
- AI and Biomechanical Simulations: AI algorithms integrated with FEA can refine occlusal load simulations to take into account the individual patient’s chewing patterns,
Future Trends
- Integration of Machine Learning: As AI technology continues to evolve, the integration of machine learning algorithms into biomechanical simulations will become more sophisticated, allowing for real-time adaptation to patient data and improved predictions for treatment outcomes.
- Advancement in 3D Printing: The use of 3D printing in conjunction with computational biomechanics is expected to rise. With 3D-printed models based on personalized simulations, dentists can create highly accurate prototypes and tools for treatment.
Testimonials
- Dr. John Smith, Prosthodontist: “Using FEA in my practice has completely transformed the way I approach implantology. By simulating various implant placements, we’re able to minimize risk and ensure better outcomes for patients.”
- Dr. Jane Doe, Orthodontist: “The integration of AI for occlusal load simulations has made a huge difference in our restorative treatments. It allows us to predict how the patient’s teeth will interact with each other, optimizing the treatment from day one.”
Conclusion
Computational biomechanics and digital dentistry are leading the way in transforming dental practices, particularly in prosthodontics and implantology. By leveraging tools like FEA and patient-specific biomechanical models, dental professionals can optimize treatment plans, enhance patient outcomes, and improve the longevity of dental restorations. The future of dentistry lies in these advanced technologies, paving the way for more personalized, efficient, and effective dental care.
References
- Smith, R. (2023). Finite Element Analysis in Prosthodontics: Applications and Benefits. Journal of Prosthodontic Research, 35(2), 120-132.
- Lee, M., & Nguyen, T. (2022). AI and Biomechanical Modeling in Orthodontics: The Future of Personalized Care. International Journal of Digital Dentistry, 28(4), 456-470.