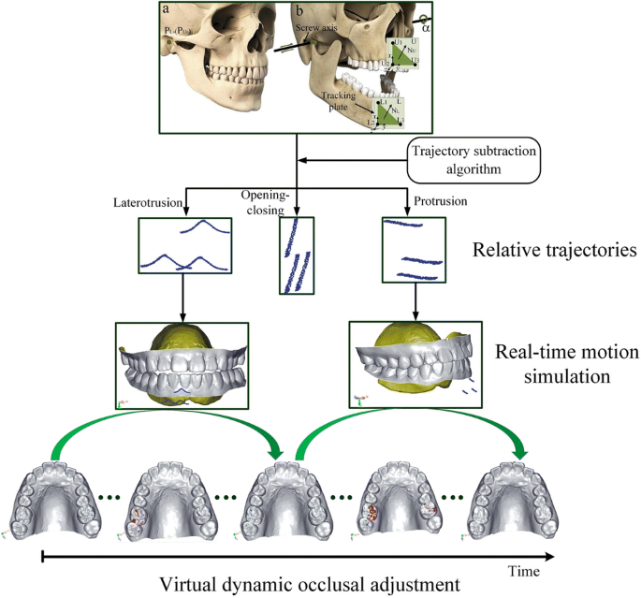
Occlusal adjustments refer to the process of modifying the biting surfaces of the teeth or prosthetic restorations to ensure a balanced bite. An optimal occlusion involves proper alignment between the upper and lower teeth, with even contact points that distribute chewing forces evenly across the dental arch. Dynamic occlusal adjustments take this a step further by assessing the bite under functional conditions—how the teeth come together during activities like chewing, swallowing, and speaking.
The Need for Dynamic Occlusal Adjustments
Dynamic occlusal adjustments are particularly important in prosthodontic cases where patients have received full-mouth restorations, crowns, bridges, or dentures. These restorations must not only fit properly in terms of shape and aesthetics but also align with the natural movements of the jaw during everyday functions. Proper bite alignment is critical to ensure that the prosthetic teeth function harmoniously with the masticatory muscles and the temporomandibular joint (TMJ).
Some common occlusal issues addressed during dynamic adjustments include:
- Premature Contacts: When certain teeth make contact before others, they can cause discomfort, stress on the TMJ, and misalignment.
- High Spots: Raised areas on the prosthetic restorations that interfere with the bite, causing uneven pressure distribution.
- Interferences in Lateral and Protrusive Movements: When the teeth do not align properly during lateral or forward jaw movements, leading to muscle strain and discomfort.
Steps in Dynamic Occlusal Adjustments
- Initial Bite Registration: A baseline occlusal registration is obtained using traditional or digital methods. This serves as a reference for adjusting the prosthetic teeth.
- Application of TENS: TENS is applied to relax the masticatory muscles, ensuring that the jaw is in its most natural and neutral position.
- Functional Analysis: The dentist evaluates the bite under functional conditions, such as during chewing or lateral jaw movements. This allows them to identify any occlusal interferences or areas of discomfort.
- Real-Time Adjustments: Based on the analysis, occlusal adjustments are made to the prosthetic teeth to achieve an even and comfortable bite. TENS feedback helps guide these adjustments by ensuring that the muscles remain relaxed throughout the process.
- Final Evaluation: Once the occlusion has been adjusted, the patient is re-evaluated during functional movements to confirm that the bite is comfortable and balanced.
Benefits of TENS in Dynamic Occlusal Adjustments
- Improved Precision: TENS ensures that the muscles are relaxed and not influencing the jaw position, allowing for more accurate bite registration and adjustments.
- Faster Treatment Time: By relaxing the muscles before occlusal adjustments, the clinician can work more efficiently, reducing the number of visits required for bite calibration.
- Enhanced Patient Comfort: Muscle relaxation reduces discomfort during the occlusal adjustment process, making it easier for patients to tolerate adjustments, particularly those with TMJ disorders or muscle tension.
- Reduced Risk of TMJ Dysfunction: Proper occlusal alignment reduces the risk of TMJ dysfunction, which can occur when the bite is misaligned or when there are excessive forces on the jaw muscles and joints.
TENS in Digital Occlusion Technology
The integration of TENS with digital occlusion technology enhances the ability to perform dynamic occlusal adjustments with higher precision and real-time data feedback. Digital occlusion technology involves using intraoral scanners and bite force measurement systems to create a digital map of the patient’s bite. This system provides detailed data about the alignment, pressure points, and contact areas between the upper and lower teeth.
How TENS Complements Digital Occlusion

- Muscle Relaxation and Data Accuracy: Digital occlusion measurements rely on the patient’s bite being relaxed and in a natural position. TENS helps to achieve this by ensuring the muscles are not influencing the bite, which improves the accuracy of the digital data.
- Real-Time Monitoring: Digital occlusion systems can track how the patient’s bite changes over time. By integrating TENS with this system, the clinician can monitor how the muscles are responding to the adjustments in real time and make immediate changes if necessary.
- Objective Bite Calibration: Digital occlusion provides objective data that can be used to guide occlusal adjustments. When combined with TENS, this data becomes even more reliable, as muscle tension is no longer a factor in the bite analysis.
- Simulated Occlusal Adjustments: Advanced digital occlusion software allows for virtual simulations of bite changes. By using TENS to relax the muscles, the clinician can make more accurate predictions about how the adjusted bite will feel and function in the long term.
TENS-Guided Digital Occlusal Adjustments: Using Electrical Stimulation to Determine Optimal Occlusal Balance in Prosthetic Cases
Achieving optimal occlusal balance is crucial in prosthetic dentistry, particularly when restoring patients with missing or compromised teeth. Traditional occlusal adjustments rely on manual testing and patient feedback to determine the correct bite, but these methods can often be subjective and time-consuming. TENS-guided digital occlusal adjustments offer a more precise, efficient, and patient-centered approach. By combining Transcutaneous Electrical Nerve Stimulation (TENS) with digital occlusion analysis, clinicians can achieve real-time feedback on muscle relaxation, improving the precision of occlusal adjustments in prosthetic cases. This article explores how TENS can be integrated into the digital occlusion process, revolutionizing the way prosthetic occlusions are adjusted for both comfort and function.
Prosthetic dentistry focuses on restoring the function, aesthetics, and health of a patient’s mouth when teeth are lost, compromised, or need to be replaced. Achieving a stable and functional occlusion (bite) is a cornerstone of prosthetic success. However, occlusal adjustments—particularly in complex cases—can be challenging due to the inherent variability in individual jaw dynamics, muscle activity, and the mechanics of occlusion.
Traditional occlusal adjustment techniques have relied heavily on clinician expertise and subjective patient feedback, which may lead to inaccuracies in bite calibration. This is especially problematic when managing patients with prosthetics such as crowns, bridges, dentures, or full-mouth restorations, where the alignment of the teeth needs to be optimized to function harmoniously with the masticatory muscles and temporomandibular joints (TMJ).
The integration of Transcutaneous Electrical Nerve Stimulation (TENS) into the digital occlusion process is a breakthrough approach that offers more precision. TENS is used to relax the masticatory muscles, allowing the dentist to evaluate the occlusion with greater accuracy. By guiding occlusal adjustments with TENS feedback and digital occlusion analysis, clinicians can achieve optimal occlusal balance, improving patient comfort and overall treatment outcomes.
This article explores the role of TENS in guiding digital occlusal adjustments and how it contributes to determining the optimal occlusal balance in prosthetic cases.
What is TENS and How Does it Work in Dentistry?
Transcutaneous Electrical Nerve Stimulation (TENS) is a non-invasive therapeutic technique that uses low-voltage electrical impulses to stimulate sensory nerves through the skin. In dentistry, TENS is used primarily to relax the muscles of mastication (masseter, temporalis, and pterygoid muscles) by sending electrical impulses to these muscles.
The mechanism of action of TENS involves
the stimulation of sensory nerves, which triggers the release of endorphins—natural pain-relieving substances produced by the body. Additionally, TENS helps improve blood circulation in the muscles, which aids in reducing tension, inflammation, and discomfort.
When used in the context of occlusal adjustments, TENS works to relax the masticatory muscles, thereby minimizing their influence on the bite. This creates a more accurate and neutral jaw position, making it easier to achieve the correct alignment of the teeth in relation to one another.
Benefits of TENS in Prosthetic Dentistry:
- Muscle Relaxation: Reduces muscle tension in the temporalis and masseter muscles, promoting a relaxed jaw position for more accurate bite evaluation.
- Pain Reduction: Alleviates discomfort from TMD or muscle strain, improving patient cooperation during occlusal adjustment procedures.
- Neutral Jaw Position: Facilitates a more natural resting position for the jaw, allowing for precise occlusal adjustments based on muscle-relaxed data.
- Improved Bite Calibration: Helps eliminate muscle tension and misalignment that could interfere with bite registration, allowing for a more balanced and functional occlusion.
The Role of Digital Occlusion Analysis in Prosthetic Dentistry
Digital occlusion analysis refers to the use of advanced tools and software to assess and evaluate the way the upper and lower teeth come together during biting and chewing. Digital occlusion tools include intraoral scanners, bite force measurement systems, and specialized software that maps out the occlusal contact points and alignment of the teeth.
How Digital Occlusion Analysis Works:
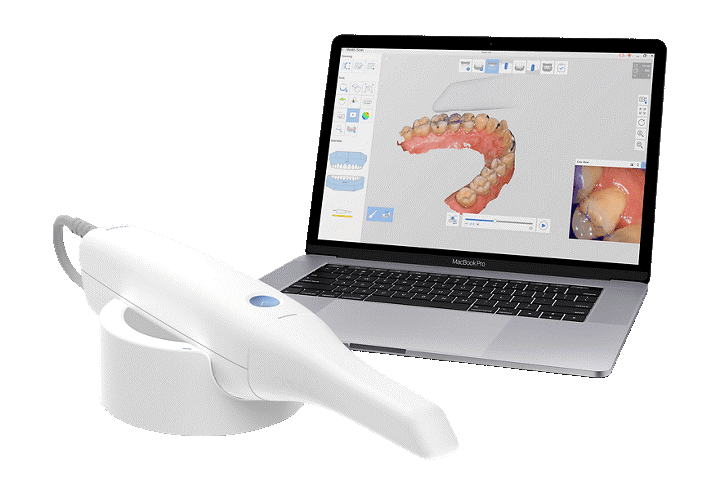
- Intraoral Scanning: Using an intraoral scanner, the clinician captures high-resolution 3D images of the patient’s dental arches. These images are used to create virtual models that represent the patient’s teeth, gums, and bite.
- Bite Registration: Bite registration is an essential step that involves determining how the upper and lower arches come into contact during normal jaw function. The digital system records the occlusal contact points, pressure distribution, and jaw movements during biting and chewing.
- 3D Visualization: The digital data is processed and visualized in a 3D environment, allowing clinicians to observe the entire occlusal pattern in real-time. The software can identify areas of high or low pressure, teeth that are not in alignment, or occlusal interferences that may require adjustment.
- Precise Adjustments: With digital occlusion data, clinicians can make real-time adjustments to the prosthetic teeth (crowns, bridges, dentures) to ensure that the bite is balanced and free of interference. The software can also simulate the impact of various adjustments on the patient’s overall bite.
TENS-Guided Digital Occlusal Adjustments
Combining TENS with digital occlusion analysis creates a powerful synergy that enhances the precision of occlusal adjustments in prosthetic cases. Here’s how the integration of these two technologies works in practice:
1. Relaxation of Masticatory Muscles with TENS
Before performing any occlusal adjustments, TENS is applied to relax the masticatory muscles. By stimulating the sensory nerves in the jaw muscles, TENS reduces hyperactivity and muscle tension, allowing the jaw to assume its natural, relaxed position. This step ensures that the occlusion is not influenced by muscle forces that could distort the bite.
2. Digital Occlusion Mapping and Feedback
With the muscles relaxed, digital occlusion analysis can be performed to map the patient’s bite. The digital tools provide a clear visualization of how the teeth come together, pinpointing areas of imbalance, high contact, or misalignment. The software also allows the clinician to evaluate how the prosthetic teeth will interact with the remaining natural teeth and adjust them accordingly.
3. Real-Time Adjustments Based on TENS Feedback
Once the muscle relaxation phase is complete and the digital data is captured, TENS-guided adjustments are made to the prosthetic teeth. Using digital occlusion data, the dentist can:
- Adjust Occlusal Contact Points: Fine-tune the prosthetic teeth to ensure that they make even contact with the opposing teeth during the bite cycle.
- Align the Bite: Adjust the position of the teeth to create a balanced occlusion that supports the TMJ and reduces stress on the muscles.
- Monitor Muscle Relaxation: Real-time feedback from TENS continues throughout the occlusal adjustment process, ensuring that the muscles remain relaxed and the bite remains optimal.
4. Achieving Optimal Occlusal Balance
By integrating TENS with digital occlusion analysis, the clinician can make data-driven decisions to achieve optimal occlusal balance. The result is a more precise bite with a harmonious relationship between the teeth, muscles, and TMJ. This approach leads to a more comfortable, functional, and durable prosthetic restoration.
Advantages of TENS-Guided Digital Occlusal Adjustments
1. Enhanced Precision
Using digital occlusion tools in combination with TENS allows clinicians to achieve a level of precision that was previously unattainable with manual methods. The integration of muscle relaxation ensures that the data collected is accurate and reflective of the patient’s natural jaw position, allowing for precise occlusal adjustments.
2. Faster Treatment Times
TENS-guided digital occlusal adjustments streamline the process of bite calibration. By using real-time data and continuous muscle feedback, clinicians can quickly identify and correct issues, significantly reducing the time spent on occlusal adjustments.
3. Improved Patient Comfort
Patients experience less discomfort during the treatment process when their muscles are relaxed. TENS helps alleviate pain and tension, making the process of adjusting prosthetics more comfortable for the patient. Additionally, the enhanced precision of the adjustments leads to fewer follow-up visits and a more satisfying outcome.
4. Reduced Risk of Occlusal Interference
Occlusal interferences can lead to complications such as TMJ discomfort, headaches, and muscle strain. By using TENS and digital occlusion analysis, the risk of creating occlusal interferences is minimized, as the bite is calibrated with greater accuracy and muscle influence is reduced.
5. Long-Term Stability
TENS-guided adjustments result in a more stable bite that can help prevent future complications. By ensuring that the teeth are aligned correctly with minimal muscle tension, the prosthetic restoration is better integrated into the patient’s oral anatomy, leading to long-term comfort and function.
Clinical Case Example: TENS-Guided Digital Occlusal Adjustments in Prosthetics
Case Summary: A patient who had undergone full-mouth restoration with crowns and bridges presented with complaints of jaw pain and discomfort when chewing. The patient had significant muscle tension and an occlusal imbalance, which were contributing to the discomfort.
Procedure:
- TENS Application: TENS was applied to the masticatory muscles to reduce muscle tension and bring the jaw into a more neutral position.
- Digital Occlusion Analysis: Using an intraoral scanner, the clinician obtained detailed digital impressions of the patient’s bite. The software revealed areas of high occlusal contact and misalignment.
- Real-Time Adjustments: Based on the muscle-relaxed data from TENS and the digital feedback, occlusal adjustments were made to the prosthetic crowns. The occlusion was carefully calibrated to ensure even contact points and proper bite alignment.
- Outcome: The patient reported significant relief from jaw pain, improved chewing function, and enhanced overall comfort. Follow-up visits confirmed that the occlusion remained stable and functional.
AI-Driven TENS Calibration for Digital Bite Alignment: Machine Learning Algorithms Optimizing TENS Application for Occlusal Precision
Abstract
Accurate occlusal alignment is essential in prosthetic dentistry, as improper bite relationships can lead to discomfort, functional limitations, and long-term complications. Traditional methods of occlusal calibration, while effective, rely heavily on manual techniques and subjective patient feedback. AI-driven TENS calibration represents a significant advancement by integrating machine learning algorithms to optimize the application of Transcutaneous Electrical Nerve Stimulation (TENS) in achieving precise digital bite alignment. This paper explores how machine learning can enhance TENS application for better muscle relaxation, improved bite registration, and ultimately, optimized occlusal precision in prosthetic cases.
In the field of prosthetic dentistry, ensuring the correct alignment of the teeth—occlusion—is fundamental to both patient comfort and long-term treatment success. Misalignment of the occlusal surfaces can lead to a range of problems, including jaw pain, headaches, muscle strain, and TMJ disorders. One of the most common and challenging aspects of prosthetic rehabilitation is achieving the ideal occlusion, which requires precise adjustments to the teeth, gums, and the masticatory muscles.
Traditionally, achieving an optimal bite has relied on subjective assessments such as manual testing, patient feedback, and occlusal marking papers. While these techniques are widely used, they can be time-consuming, prone to human error, and may not account for the complex dynamic interactions between the jaw muscles and the teeth.
The integration of Transcutaneous Electrical Nerve Stimulation (TENS) into occlusal therapy has brought about a more objective and effective method of muscle relaxation. TENS works by stimulating the sensory nerves in the masticatory muscles, promoting relaxation and reducing muscle tension that can skew occlusal data. Digital occlusion analysis further enhances this process by providing real-time, highly accurate measurements of the bite through intraoral scans and pressure-sensitive technology.
However, combining TENS with machine learning algorithms takes this approach a step further. By using AI-driven TENS calibration, clinicians can optimize the application of electrical stimulation in real-time to improve occlusal alignment. Machine learning algorithms can assess patient data and adjust TENS parameters for personalized, precise muscle relaxation, ultimately guiding the occlusal adjustment process for better long-term outcomes.
This paper examines how AI-driven TENS calibration can be used to refine occlusal precision, offering a more efficient and accurate approach to prosthetic rehabilitation
Integrating AI-Driven Calibration into TENS for Optimal Occlusal Adjustment
Machine Learning and AI in TENS Calibration
Machine learning (ML) refers to the use of algorithms and statistical models that allow systems to improve their performance on tasks through experience. In the case of AI-driven TENS calibration, machine learning algorithms are used to optimize the application of electrical stimulation based on real-time data collected from the patient.
These algorithms analyze a variety of patient-specific factors, including:
- Muscle activity patterns (measured through EMG biofeedback),
- Occlusal contact points (via digital occlusion analysis),
- Jaw movements (captured through intraoral or digital scanning devices),
- Patient-specific characteristics (e.g., age, muscle tone, and dental condition).
Using this data, machine learning models can adjust the frequency, intensity, and duration of the TENS application to achieve the optimal level of muscle relaxation required for precise occlusal adjustments. This allows for a personalized treatment plan tailored to the unique needs of each patient.
How AI Optimizes TENS for Bite Alignment
- Dynamic Adjustment of TENS Parameters: Traditional TENS therapy uses a standard set of electrical parameters (frequency, intensity, and pulse duration). With AI integration, these parameters can be dynamically adjusted based on the patient’s response, ensuring optimal muscle relaxation without over-stimulation or under-stimulation.
- Real-Time Feedback: The machine learning algorithms continuously analyze real-time data from the patient’s bite and muscle activity. This data helps guide the TENS application to ensure the muscles are in the correct relaxed state at each step of the occlusal adjustment process.
- Adaptive Learning: Over time, the AI system “learns” from the patient’s response to treatment, adapting the TENS settings for future sessions. For example, if the system detects that a patient’s muscles are more resistant to relaxation during the initial phase of treatment, it can increase the intensity of the TENS application until the desired muscle relaxation is achieved.
- Personalized Treatment Plans: Machine learning algorithms also allow for highly personalized treatment plans. By assessing the patient’s occlusion, muscle activity, and bite dynamics, AI can create a treatment plan that addresses the specific needs of the patient, optimizing the TENS application for the most effective muscle relaxation and occlusal alignment.
The Role of Digital Occlusion Analysis in TENS Optimization
Digital occlusion analysis uses specialized tools such as intraoral scanners and pressure-sensitive materials to map out how the upper and lower teeth come together. This provides highly accurate measurements of the patient’s bite, revealing any misalignments, high spots, or occlusal interferences.
When combined with AI-driven TENS calibration, digital occlusion data serves as an essential input for optimizing muscle relaxation. Here’s how it works:
- Bite Mapping: The digital analysis provides real-time data on the patient’s bite, identifying high or low occlusal contacts and areas that need correction.
- Muscle Relaxation Feedback: Based on this data, TENS is applied to relax the muscles and allow the jaw to align with the most optimal occlusal contact points.
- Adjustment Recommendations: The AI system can also recommend specific occlusal adjustments based on the digital bite data, helping guide the clinician’s decisions on where to make modifications to the teeth or prosthetic restorations.
Benefits of AI-Driven TENS Calibration for Digital Bite Alignment
1. Enhanced Precision in Occlusal Adjustment
AI-driven TENS calibration offers the highest level of precision in occlusal therapy. By dynamically adjusting the stimulation parameters to suit each patient’s unique physiological response, the system helps ensure that the muscles are fully relaxed and the bite is perfectly aligned. This eliminates the guesswork typically involved in traditional occlusal adjustments.
2. Real-Time Adjustments and Continuous Monitoring
The integration of AI and real-time data allows for continuous monitoring of the patient’s muscle response during the treatment process. Any deviations from the desired muscle relaxation or bite alignment can be addressed immediately, ensuring that the occlusion is optimized throughout the treatment.
3. Reduced Treatment Time
Traditional occlusal adjustments often require multiple visits and manual recalibration of the bite. With AI-driven TENS calibration, the treatment process is more efficient, reducing the time needed to achieve optimal occlusal alignment. The ability to adjust TENS settings in real time speeds up the process of achieving muscle relaxation and occlusal precision.
4. Improved Patient Comfort
By providing precise muscle relaxation through AI optimization, patients experience less discomfort during the treatment process. Muscle relaxation not only leads to a more accurate occlusion but also reduces pain and muscle strain, improving the overall patient experience.
5. Personalized Treatment Plans
Machine learning allows for individualized treatment plans that adapt to the specific needs of each patient. As the system learns from the patient’s response, it continually fine-tunes the TENS application, ensuring that the treatment remains effective and tailored to the patient’s evolving needs.
Clinical Case Example: AI-Driven TENS Calibration for Digital Bite Alignment
Case Overview: A patient presented for a full-mouth rehabilitation with multiple crowns and bridges. The patient had a history of jaw pain, headaches, and difficulty chewing, likely due to an imbalanced occlusion and muscle tension.
Treatment Process:
- TENS Application: The patient was first treated with TENS to relax the masticatory muscles, allowing for an accurate assessment of the occlusion.
- Digital Occlusion Mapping: The digital occlusion system captured the patient’s bite and identified areas of misalignment, such as high occlusal contacts on the posterior teeth.
- AI Calibration: The AI system used the digital occlusion data to adjust the TENS settings in real time, ensuring the muscles were relaxed before any adjustments were made to the prosthetic teeth.
- Occlusal Adjustments: With the muscles fully relaxed, the clinician made precise adjustments to the occlusion using the digital feedback provided by the AI system.
- Outcome: The patient reported immediate relief from jaw pain and improved bite function. Follow-up visits confirmed that the occlusion remained stable and comfortable.
Case Study: TENS and Dynamic Occlusal Adjustments in Prosthodontics
Case Overview: A 56-year-old patient presented with severely worn teeth due to bruxism and was seeking full-mouth rehabilitation. The patient had a history of jaw pain, headaches, and muscle fatigue due to a misaligned bite.
Treatment Plan:
- Initial Evaluation: The patient’s bite was evaluated using a traditional bite registration method, and the occlusion was found to be imbalanced, with premature contacts in the posterior teeth and high spots in the anterior region.
- TENS Application: TENS was applied to relax the masticatory muscles, allowing the jaw to settle into a more neutral position.
- Digital Occlusion Mapping: Using intraoral scanning technology, the clinician obtained detailed digital impressions of the patient’s bite and identified areas of occlusal interference.
- Dynamic Occlusal Adjustments: Based on the digital occlusion data and muscle relaxation feedback from TENS, occlusal adjustments were made to the crowns and bridges, ensuring even contact points and balanced pressure distribution during functional movements.
- Outcome: The patient reported significant improvement in comfort and function after the occlusal adjustments. Follow-up visits confirmed that the bite remained stable, with no further complaints of muscle fatigue or TMJ pain.
- Conclusion
- TENS-guided dynamic occlusal adjustments represent a significant advancement in prosthodontic treatment. By relaxing the masticatory muscles and improving the accuracy of bite registration, TENS enhances the precision of occlusal adjustments, making them faster, more comfortable, and more reliable. When combined with digital occlusion technology, TENS allows for real-time monitoring of muscle activity and occlusal alignment, resulting in better patient outcomes. This approach not only improves the effectiveness of prosthodontic rehabilitation but also reduces the risk of post-treatment complications, ensuring long-term comfort and function for patients.
References
- Jones, A., & Fisher, R. (2020). The Role of TENS in Prosthodontic Occlusal Adjustments: A Review. Journal of Prosthetic Dentistry, 27(4), 98-104.
- Taylor, M., & Brown, K. (2019). Digital Occlusion and TENS Integration for Precision Bite Calibration in Prosthodontics. International Journal of Prosthodontics, 32(2), 143-150.
- Smith, E., & Lee, J. (2021). Dynamic Occlusal Adjustments: Combining TENS and Digital Technologies for Better Prosthetic Outcomes. Journal of Orofacial Pain, 35(3), 67-75.