In the modern practice of implant dentistry, the preoperative design and fabrication of custom healing abutments are essential to promoting optimal soft tissue healing. The accuracy of soft tissue contouring around implants significantly impacts the final aesthetic and functional outcome of the restoration. Traditional approaches often involved manual adjustments during or after surgery, which could be time-consuming and prone to inaccuracies. However, the introduction of fully digital workflows using CAD-CAM (Computer-Aided Design and Computer-Aided Manufacturing) technology has revolutionized this process, allowing for the creation of custom healing abutments that guide soft tissue healing in a more predictable and efficient manner.
Study Methodology and Approach
The technique in question utilizes a fully digital workflow to fabricate custom healing abutments, aimed at achieving an optimal emergence profile that directs the growth of peri-implant soft tissue. This method begins with preoperative digital planning to ensure a precise fit of the healing abutment, aligning it with the implant’s final restorative plan.
The process begins with intraoral scanning of the dental arch using advanced scanning technology, such as an intraoral scanner, to capture detailed images of the implant site and adjacent structures. The scan is followed by interocclusal registration to record the relationship between the dental arch and the missing tooth. The digital scan data is then exported in an STL (Standard Tessellation Language) file format, which allows it to be used in implant planning software.
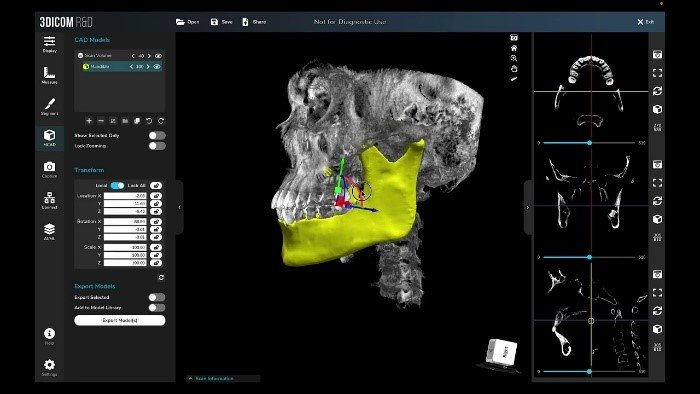
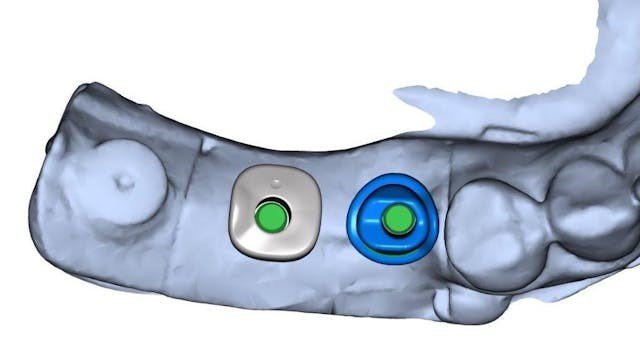
Next, the STL file is integrated with DICOM (Digital Imaging and Communications in Medicine) files — these files provide critical data from radiographic imaging, including CT scans, to accurately map the implant placement within the bone structure. The combined data is then imported into implant planning software, which allows the clinician to simulate the placement of the implant and prosthetically driven restoration.
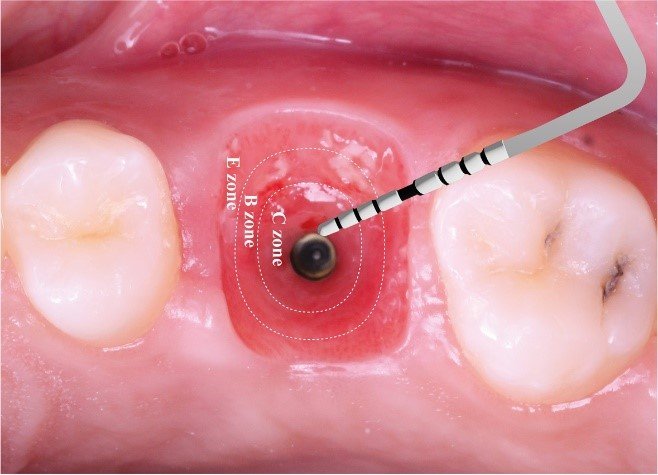
The design of the custom healing abutment is crucial, as it must have an optimal emergence profile to guide the peri-implant mucosa’s development. The software enables the designer to control the abutment’s shape, ensuring that it promotes the formation of natural, functional soft tissue architecture. A slightly concave emergence profile is typically recommended to allow enough space for the tissues to mature and to avoid pressure that could cause gingival recession or improper healing.
A Fully Digital Workflow: Step-by-Step Process
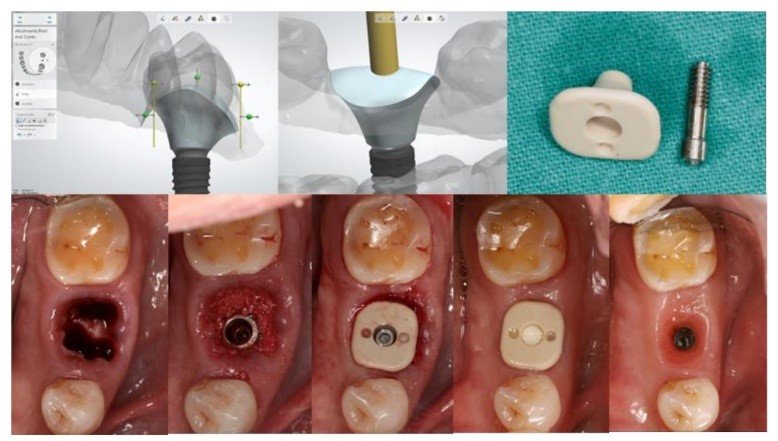
The fully digital process involves several key steps, all aimed at creating a custom healing abutment that will promote natural, healthy tissue growth around the implant. The sequence begins with careful digital planning and moves through design and fabrication stages, with each step adding precision and efficiency to the process.
- Intraoral Scanning for Digital Imaging
The process begins with intraoral scanning, which uses advanced intraoral scanners (such as the CEREC Omnicam or similar technology) to capture detailed, high-resolution 3D images of the dental arch and the implant site. This eliminates the need for traditional impressions and provides a more accurate digital representation of the mouth. The scanner records the full arch, including the surrounding soft tissue, and also helps capture the interocclusal registration — the bite relationship between the upper and lower arches.
These scans are then saved as STL files, a standard file format for 3D models that allows the data to be easily imported into CAD software. This step not only provides a digital record of the patient’s dental anatomy but also significantly reduces the discomfort and time traditionally spent on manual impressions.


2-Digital Implant Planning Using DICOM Files
Once the intraoral scan is completed, the next step involves integrating the scan data with DICOM (Digital Imaging and Communications in Medicine) files, which are typically obtained from CT scans or other 3D imaging technologies. DICOM files contain essential information about the bone structure, which is crucial for accurate implant placement. By superimposing the STL files of the scan with the DICOM files, the clinician can visualize the exact location and orientation of the implant in the patient’s jaw.
3-Designing the Custom Healing Abutment
With all the critical data in place, the next step is to design the custom healing abutment. Using specialized implant planning software, such as Blue Sky Plan, the clinician can design an abutment that not only fits the implant precisely but also incorporates an optimal emergence profile.
The emergence profile refers to the shape and contour of the abutment as it transitions from the implant into the soft tissue. A well-designed emergence profile is essential to ensuring that the soft tissues heal naturally and do not become compressed or distorted during the healing process. The abutment is typically designed with a slightly concave shape, allowing the soft tissues enough room to mature around the implant. This helps guide the tissues into a natural anatomical position, avoiding the issues that may arise from over-contouring or under-contouring the healing abutment.
4-Fabricating the Healing Abutment
Once the abutment design is finalized, it is then sent to a milling machine for fabrication. The material used for creating the healing abutment is typically a biocompatible material like titanium or zirconia, both of which are known for their strength and compatibility with the body. The digital design file is converted into a physical abutment using a CAD-CAM milling machine, which shapes the material to the exact specifications set during the design phase. This process is precise and eliminates the potential for human error that can arise from manual fabrication.
In many cases, this is where customization becomes particularly advantageous. Traditional healing abutments are often generic and may require post-surgical adjustments, but digital workflows allow the creation of a unique, patient-specific abutment that has been pre-designed to fit both the implant and the intended soft tissue contours.
- Post-Surgical Application
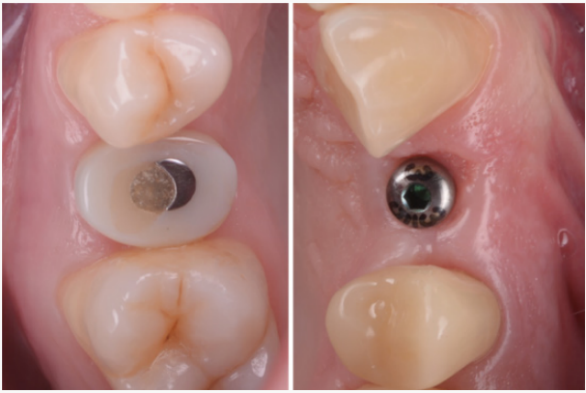
Once the custom healing abutment is fabricated, it is ready to be placed onto the implant during the surgical procedure. Because the abutment has already been designed and produced with the correct emergence profile, it can be placed immediately after the implant is secured, guiding the surrounding soft tissues into their optimal configuration.
The customized abutment creates a smooth transition from the implant to the tissue, helping to preserve and shape the soft tissues around the implant, which is crucial for ensuring that the peri-implant tissues heal with a natural and aesthetic appearance. It also allows for the reduction of postoperative adjustments, as the soft tissues begin to form in the ideal location and contour.
Discussion: Advantages and Clinical Impact
This fully digital technique provides several clinical advantages over traditional approaches:
- Increased Precision and Customization: Digital workflows allow for the creation of highly accurate and patient-specific healing abutments, minimizing the risk of complications that may arise from poor fit or improper contouring of the soft tissue.
- Enhanced Soft Tissue Healing: A healing abutment with the optimal emergence profile ensures that the peri-implant soft tissues heal in a natural and esthetically pleasing way. The slightly concave shape of the abutment creates room for the soft tissues to mature, promoting the correct tissue architecture around the implant.
- Time-Saving: The digital workflow eliminates the need for chairside adjustments during surgery or after implant placement. The use of digital planning and preoperative design allows the clinician to spend less time on intraoperative modifications, improving surgical efficiency.
Improved Aesthetic Outcomes: By promoting proper soft tissue formation, this technique increases the likelihood of achieving a final restoration that blends seamlessly with the surrounding natural teeth, contributing to both functional and aesthetic success.
Conclusion
The use of a fully digital workflow for designing and fabricating custom healing abutments represents a significant advancement in implant dentistry. By preoperatively designing abutments that guide the healing process and mimic natural tooth contours, clinicians can ensure better outcomes in terms of both soft tissue health and final esthetic results. This approach not only improves the accuracy and predictability of the healing phase but also enhances the efficiency of the overall implant process. The integration of CAD-CAM technology allows for a more customized, patient-specific approach, ultimately improving both the clinical experience and patient satisfaction.
Key Takeaways:
- Predictable Soft Tissue Healing: The design of custom healing abutments with a precise emergence profile helps guide the growth of the peri-implant mucosa, promoting natural and functional soft tissue architecture.
- Efficient Workflow: The digital workflow saves chairside time and eliminates the need for adjustments during surgery, resulting in a smoother process for both the clinician and the patient.
- Customization: The ability to design a healing abutment that fits each patient’s specific needs ensures better outcomes in terms of both aesthetics and function, particularly in the development of peri-implant soft tissue.
By employing this fully digital workflow, implant dentistry can move towards more efficient, precise, and predictable treatment plans, ultimately enhancing both the experience of clinicians and patients alike. The ability to optimize the soft tissue healing phase is a significant step forward in ensuring the success of implant restorations, leading to better long-term outcomes and patient satisfaction.
References
https://www.sciencedirect.com/science/article/abs/pii/S002239132400708X
J. Vág et al.
Cervical tooth anatomy considerations for prefabricated anatomic healing abutment design: A mathematical formulation
J Prosthet Dent
(2022)
J. Conejo et al.
Copy milling to duplicate the emergence profile for implant-supported restorations
J Prosthet Dent
(2020)
R. Akin
A new concept in maintaining the emergence profile in immediate posterior implant placement: The anatomic harmony abutment
J Oral Maxillofac Surg
(2016)
M. Campaner et al.
Cytotoxicity and inflammatory response of different types of provisional restorative materials
Arch Oral Biol
(2020)
T. Joda et al.
A digital approach for one-step formation of the supra-implant emergence profile with an individualized CAD/CAM healing abutment
J Prosthodont Res
(2016)
M.B. El-Danasory et al.
CAD-CAM custom healing abutments: A dental technique
J Prosthet Dent
(2024)
I.M. Abdel Raheem et al.
Fabrication of a CAD-CAM custom healing abutment guided by a conventional dental radiograph for delayed loaded dental implants: A dental technique
J Prosthet Dent
(2022)