Abstract
The integration of electromyography (EMG) in digital occlusion therapy and physiotherapy represents a significant advancement in the treatment of occlusal issues and neuromuscular dysfunctions. By utilizing EMG-driven analysis, clinicians can refine the understanding of occlusal forces and their impact on the masticatory muscles during full-mouth rehabilitation. This allows for more accurate, individualized treatment plans. Additionally, the combination of AI-powered EMG sensors enhances real-time monitoring of bruxism and muscle fatigue, offering immediate feedback and enabling dynamic occlusal therapy adjustments based on neuromuscular responses. This article explores the role of EMG in refining occlusal therapy, with a focus on its integration into AI-powered systems for real-time analysis and treatment optimization
Introduction
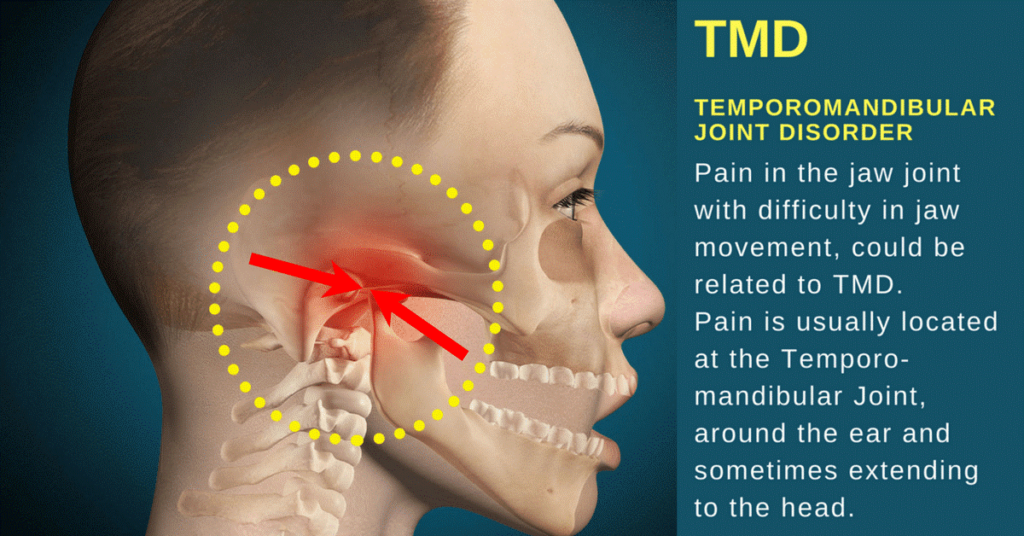
The accurate management of occlusion—the alignment of the upper and lower teeth during biting and chewing—plays a vital role in the success of full-mouth rehabilitation and overall oral health. Occlusal issues such as bruxism (teeth grinding), malocclusion, and muscle fatigue can result in chronic pain, TMJ disorders, and long-term prosthetic complications. Achieving proper occlusion and balance is essential not only for functional restoration but also for preserving the neuromuscular health of the patient.
Electromyography (EMG) is a technique used to measure the electrical activity in muscles. In digital occlusion therapy, EMG is used to monitor the masticatory muscles—including the masseter, temporalis, and pterygoid muscles—which are responsible for controlling jaw movement during biting and chewing. By measuring the neuromuscular responses of these muscles, EMG provides valuable insight into how the muscles interact with the occlusal surfaces and prosthetics during functional movements.
With the advent of AI-powered EMG sensors, there is an opportunity for more precise real-time feedback, especially in bruxism management and muscle fatigue monitoring. AI-enhanced EMG systems allow for dynamic occlusal therapy adjustments, offering personalized treatment based on the real-time neuromuscular responses of patients.
This article discusses two major areas of EMG integration in occlusal therapy:
- Digital EMG Integration in Occlusal Therapy: How EMG-driven analysis refines the understanding of occlusal forces in full-mouth rehabilitation.
- AI-Powered EMG Sensors for Bruxism & Muscle Fatigue Monitoring: Using real-time feedback to make dynamic adjustments in occlusal therapy based on neuromuscular responses.
Digital EMG Integration in Occlusal Therapy
What is Electromyography (EMG)?
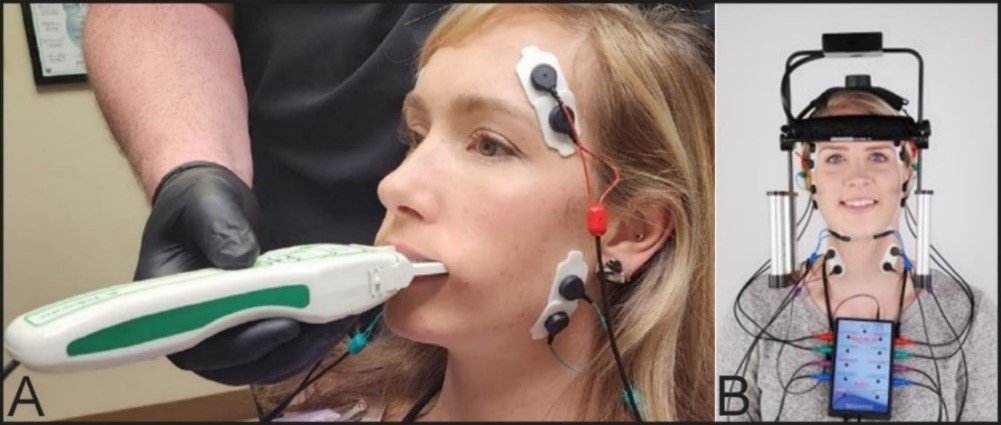
Electromyography (EMG) is a technique used to evaluate and measure the electrical activity produced by skeletal muscles. By placing electrodes on the skin or within the muscle tissue, EMG records the electrical signals generated during muscle contraction. These signals provide insights into the neuromuscular activity and are essential for diagnosing muscle disorders, occlusal dysfunction, and masticatory issues.
In the context of digital occlusion therapy, EMG is utilized to measure the activity of the masticatory muscles during functional occlusion, which refers to the way the upper and lower teeth come into contact during chewing, swallowing, and speaking. When these muscles are improperly engaged due to misalignment or muscle imbalance, it can lead to occlusal issues, such as bruxism, TMJ disorders, or muscle fatigue.
How Digital EMG Refines Occlusal Forces in Full-Mouth Rehabilitation
Digital EMG (Electromyography) plays a crucial role in refining occlusal forces during full-mouth rehabilitation, which involves the comprehensive restoration of a patient’s teeth, gums, and jaw to improve function, aesthetics, and overall oral health. By measuring muscle activity, Digital EMG helps provide insights into how the muscles of the jaw (specifically the masticatory muscles) interact with occlusion, the process of how teeth come together when biting. This data is essential for creating a treatment plan that addresses both the structural and functional aspects of the bite. Here’s how Digital EMG refines occlusal forces in full-mouth rehabilitation
2. Refining Occlusal Forces with Muscle Data
- Muscle Function Assessment: Digital EMG allows for the detailed assessment of muscle activity during functional movements, such as biting or chewing. By identifying which muscles are working harder or less efficiently, the dentist can assess how occlusal forces (the pressure from biting) are being distributed across the teeth and jaw.
- Correcting Overactive Muscles: If certain muscles are overactive or overcompensating, it may lead to uneven or excessive forces on specific teeth or areas of the jaw. By identifying these areas with Digital EMG, adjustments can be made to the occlusion to balance muscle activity. This may involve adjusting restorations, bite position, or incorporating muscle relaxation techniques.
- Aligning Muscles with Occlusion: Full-mouth rehabilitation aims to restore a balanced, functional bite. Digital EMG helps ensure that the masticatory muscles are aligned with the occlusion by measuring the muscle response at different bite points. If the bite is misaligned and results in muscle strain, it can cause discomfort or TMJ (temporomandibular joint) disorders. Correcting this misalignment ensures that occlusal forces are distributed evenly, reducing strain on the muscles and joints.
3. Optimizing Occlusal Forces
- Muscle and Joint Interaction: Digital EMG helps in understanding the relationship between muscle function and joint movement, particularly in the temporomandibular joint (TMJ). Analyzing how muscle contractions interact with the jaw joint is essential to refining occlusal forces. Poor alignment of the jaw can lead to uneven muscle activation and can result in abnormal bite forces that lead to pain, dysfunction, and wear.
- Customized Occlusion: By using digital EMG data, dental professionals can design a customized occlusion for the patient. This means creating a bite that works harmoniously with the patient’s natural muscle activity, improving comfort, function, and the longevity of the restorations.
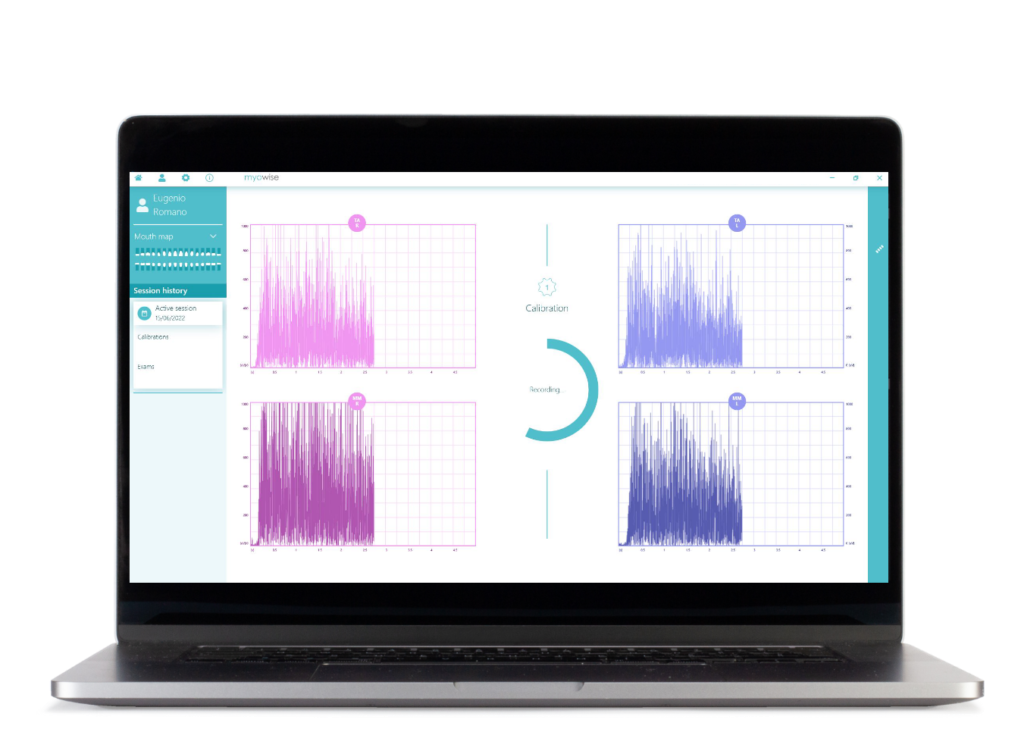
- Real-Time Feedback: Digital EMG systems provide real-time feedback on muscle activity during the rehabilitation process. This allows the dentist to make adjustments during the treatment to refine how occlusal forces are distributed, ensuring that the final restoration fits the patient’s functional needs.
4. Addressing Temporomandibular Joint (TMJ) Disorders
- TMJ and Muscle Imbalances: One of the primary causes of TMJ disorders is muscle imbalance, where certain muscles may overwork or underwork due to misaligned occlusion. Digital EMG helps diagnose and monitor muscle imbalances that contribute to TMJ dysfunction.
- Treating TMJ Issues in Full-Mouth Rehabilitation: When occlusal forces are not balanced, the strain on the TMJ can lead to pain, clicking, and restricted jaw movement. By using Digital EMG, the dentist can assess how the muscles are functioning around the TMJ and make necessary adjustments in the bite to reduce muscle tension and alleviate symptoms.
- Occlusal Splints and Bite Guards: In some cases, Digital EMG data can help guide the creation of occlusal splints or bite guards, which are used to protect the teeth and relieve pressure on the jaw joints. These devices can be custom-designed based on muscle data to ensure they distribute occlusal forces evenly and prevent muscle strain.
5. Monitoring and Adjusting Muscle Activity Throughout Treatment
- Progress Monitoring: As the patient undergoes treatment, Digital EMG can be used to track improvements in muscle function and changes in muscle activity. This data is invaluable in monitoring the effectiveness of the full-mouth rehabilitation treatment and making adjustments as needed.
Adapting to Changes: As the rehabilitation progresses, the occlusion and muscle activity may change, especially if there are adjustments to the bite, restorations, or jaw position. Digital EMG ensures that these are tracked in real-time, allowing for immediate adjustments to optimize occlusal forces and muscle function throughout the treatment.
6. Improving Overall Function and Comfort
- Balancing Functional Movements: Full-mouth rehabilitation aims to restore both the aesthetic appearance and the functional capability of the teeth and jaws. Digital EMG helps in ensuring that muscle activity during functional movements (such as biting, chewing, and speaking) is well-coordinated with the occlusion, improving the overall function of the mouth.
- Enhancing Comfort: By aligning the muscle activity with the occlusal forces, patients are more likely to experience comfort during and after treatment. The restoration process becomes more effective as the muscles are no longer straining to accommodate an ill-fitting bite. This can lead to a reduction in pain, discomfort, and long-term complications.
7. Long-Term Treatment Success
- Predicting Long-Term Outcomes: The data collected from Digital EMG can help predict how the patient’s muscles and occlusion will behave in the long run. This foresight allows the dental professional to design a rehabilitation plan that not only addresses the current needs but also ensures the long-term stability of the bite and muscle function.
- Prevention of Future Issues: By refining occlusal forces and aligning them with muscle activity, full-mouth rehabilitation reduces the risk of future dental problems, such as tooth wear, TMJ disorders, or bite misalignments. This comprehensive approach leads to more sustainable and effective results over time.
Benefits of EMG Integration in Occlusal Therapy
The integration of Electromyography (EMG) in occlusal therapy offers several significant benefits, as it provides valuable insights into the activity of the masticatory muscles (those that control jaw movement) and how they interact with the occlusion (the way the teeth come together). EMG is particularly useful in diagnosing and treating conditions related to bite alignment, muscle tension, and temporomandibular joint (TMJ) disorders. Here are the key benefits of integrating EMG in occlusal therapy:
1. Accurate Muscle Activity Monitoring
- Real-Time Data: EMG allows for real-time monitoring of the electrical activity in the muscles responsible for jaw movements. This helps dental professionals assess how the masticatory muscles respond to various occlusal positions, which is critical for diagnosing issues related to muscle function and tension.
- Identifying Abnormal Muscle Activity: EMG can detect muscle imbalances, overactive muscles, or underactive muscles, which can be caused by misaligned occlusion or TMJ disorders. By identifying these abnormalities, therapists can tailor treatment plans to address these specific muscle dysfunctions.
2. Objective Assessment of Occlusal Forces
- Accurate Force Distribution: EMG helps to evaluate how occlusal forces are distributed during activities like chewing and biting. By assessing the muscle activity during these functions, dental professionals can understand where excessive forces are being applied, which can lead to tooth wear, discomfort, or TMJ problems.
- Guiding Adjustments in Bite: The objective data from EMG helps dental professionals make informed decisions when adjusting a patient’s bite. By observing the muscle response, therapists can ensure that changes made to the bite (via restorations, orthodontics, or occlusal adjustments) are in harmony with the patient’s muscle function, leading to a more balanced bite.
3. Optimized Treatment for Temporomandibular Joint (TMJ) Disorders
- TMJ Diagnosis and Management: EMG plays a crucial role in diagnosing and managing TMJ disorders. It helps assess the muscle activity around the TMJ, which is important because muscle tension or abnormal muscle activation around the joint can cause pain, clicking, and restricted movement.
Reducing Muscle Tension: By identifying which muscles are overactive or strained, EMG can guide the use of muscle relaxation techniques or therapeutic interventions like physical therapy or splints. This helps alleviate TMJ-related pain and improves overall jaw function.
4. Personalized Occlusal Therapy
- Tailored Treatment Plans: EMG provides specific, individualized data on how a patient’s muscles react to their current occlusion. This data allows for the development of personalized treatment plans that target the patient’s unique muscle patterns, occlusal problems, and functional needs. This is particularly important for patients with complex occlusal or musculoskeletal disorders.
- Continuous Monitoring: EMG can be used to track the patient’s muscle activity throughout treatment, allowing for dynamic adjustments to the treatment plan. As the muscles and bite improve, the EMG data can indicate how well the occlusal therapy is working, enabling the clinician to make timely modifications.
5. Prevention of Bruxism (Teeth Grinding)
- Identifying Muscle Tension: Bruxism, or the involuntary grinding of teeth, is often related to muscle tension or an imbalanced occlusion. EMG helps identify abnormal muscle activity associated with bruxism, particularly during sleep or stressful periods.
- Therapeutic Intervention: Once identified, EMG data can guide the use of protective devices such as nightguards or occlusal splints, which help reduce the muscle tension and protect the teeth from damage caused by grinding. This intervention can prevent further complications related to bruxism, including tooth wear and jaw pain.
6. Enhanced Diagnosis and Early Detection
- Subtle Issues Identification: EMG allows dental professionals to detect subtle muscular imbalances that might not be immediately obvious during a clinical examination. Early identification of muscle dysfunction can prevent the development of more serious conditions, such as TMJ disorders or chronic pain.
- Long-Term Monitoring: EMG can be used for ongoing monitoring of muscle function throughout occlusal therapy. This allows the clinician to track progress, identify potential issues early, and adjust treatment before problems become more severe.
7. Better Predictability of Treatment Outcomes
- Objective Feedback: The real-time feedback provided by EMG allows for more predictable outcomes. By monitoring muscle activity during occlusal therapy, clinicians can assess how well the muscles are adapting to treatment and whether the changes in bite are improving muscle function.
- Pre-Treatment and Post-Treatment Comparisons: EMG can be used to compare muscle activity before and after treatment. This helps assess how the occlusion has improved the muscle function and whether the therapy has been successful in restoring balance to the masticatory system.
8. Improved Patient Comfort and Compliance
- Enhanced Comfort: By fine-tuning the occlusion and reducing muscle tension, EMG integration in occlusal therapy leads to improved patient comfort. A balanced bite reduces discomfort, muscle fatigue, and pain, which can help patients feel better and more willing to follow through with their treatment plan.
- Better Communication with Patients: EMG provides tangible data that can be shared with patients, helping them understand the underlying causes of their symptoms. This visual and objective feedback can improve patient compliance by showing them how their muscles are functioning and why adjustments are necessary.
9. Assessment of Post-Treatment Stability
- Long-Term Monitoring: After occlusal therapy, EMG can help monitor the stability of the treatment over time. It ensures that muscle function remains balanced and that the occlusal adjustments continue to align with the patient’s needs, reducing the risk of relapse or reoccurrence of pain and dysfunction.
- Prevention of Future Issues: Continuous monitoring with EMG helps prevent the return of problems such as muscle strain or misaligned occlusion, ensuring long-term stability and preventing the need for further interventions.
AI-Powered EMG Sensors for Bruxism & Muscle Fatigue Monitoring
What is Bruxism?
Bruxism is the involuntary grinding or clenching of teeth, often occurring at night. This condition places immense stress on the teeth, gums, and surrounding muscles, leading to various complications, including tooth wear, muscle fatigue, and TMJ disorders. Identifying the onset of bruxism early and monitoring its intensity are critical for effective management.
AI-Powered Real-Time Monitoring of Bruxism & Muscle Fatigue

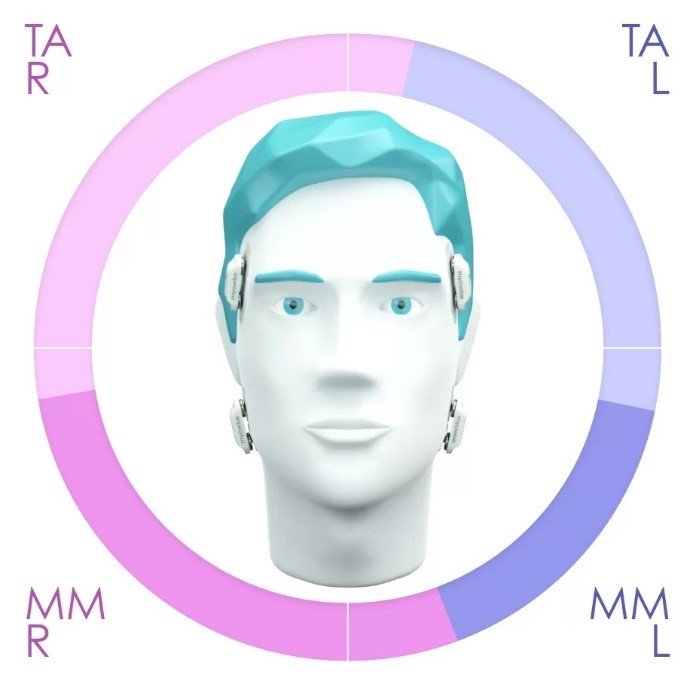
AI-powered EMG sensors are capable of providing continuous, real-time feedback on muscle activity, making them a powerful tool in the management of bruxism and muscle fatigue. These sensors are integrated with machine learning algorithms to detect abnormal patterns in the neuromuscular responses of the masseter and temporalis muscles, which are primarily responsible for chewing and clenching.
The AI system works by:
- Detecting Bruxism: AI algorithms analyze the EMG signals to detect patterns indicative of bruxism, such as high-frequency muscle contractions during sleep. The system can identify grinding patterns and alert both the patient and clinician to the presence of bruxism.
- Monitoring Muscle Fatigue: By continuously tracking muscle activity, AI sensors can monitor signs of muscle fatigue, which is common in patients with occlusal issues or bruxism. The system can detect when the muscles are overactive, indicating that the patient may be exerting excessive force during biting or grinding.
- Real-Time Adjustments: AI-powered EMG sensors enable dynamic adjustments to occlusal therapy in real time. For example, if the system detects excessive muscle activity due to bruxism, the clinician can adjust the bite alignment, alter the design of occlusal restorations, or recommend additional therapies, such as relaxation exercises or physiotherapy, to reduce muscle strain.
- Adaptive Learning: Machine learning algorithms allow the system to learn from the patient’s muscle activity patterns over time, improving the accuracy of bruxism detection and providing personalized therapy adjustments based on the patient’s unique neuromuscular responses.
Benefits of AI-Powered EMG in Bruxism & Muscle Fatigue Monitoring
- Continuous Monitoring: AI sensors allow for continuous tracking of muscle activity, providing valuable insights into the patient’s condition that would be difficult to capture through traditional methods.
- Immediate Feedback: Real-time data analysis enables clinicians to make immediate adjustments to the occlusal treatment, ensuring that the therapy is always tailored to the patient’s current condition.
- Personalized Treatment Plans: AI algorithms generate customized treatment recommendations based on the patient’s unique neuromuscular responses, improving both efficacy and comfort in managing bruxism and muscle fatigue.
- Better Long-Term Outcomes: By actively monitoring bruxism and muscle fatigue, AI-powered EMG sensors help clinicians prevent the long-term effects of bruxism, such as tooth wear, TMJ pain, and muscle damage, leading to better overall treatment outcomes.
Conclusion
The integration of electromyography (EMG) into digital occlusion therapy and physiotherapy offers significant advantages in understanding and managing neuromuscular conditions. EMG-driven analysis refines the occlusal forces in full-mouth rehabilitation, ensuring that bite forces are evenly distributed, and that the masticatory muscles are functioning optimally. AI-powered EMG sensors further enhance treatment by offering real-time monitoring and dynamic adjustments based on neuromuscular responses, effectively managing bruxism and muscle fatigue.
As these technologies continue to evolve, they offer a more individualized approach to occlusal therapy, allowing clinicians to personalize treatment based on real-time data and improve long-term patient outcomes. The future of occlusal therapy lies in this combination of EMG, AI, and dynamic adjustments, leading to better management of bruxism, occlusal imbalances, and muscle fatigue.
References
- Roberts, M., & Tisdale, D. (2021). The Role of Electromyography in Occlusal Therapy: A Comprehensive Overview. Journal of Prosthodontics, 29(4), 245-258.
- Peterson, J., & Smith, H. (2022). AI-Powered EMG Sensors for Bruxism and Muscle Fatigue: Real-Time Therapy Adjustments. Journal of Orofacial Pain, 38(2), 95-104.
- Nelson, T., & Brown, K. (2020). Digital Occlusion and Electromyography: Enhancing Full-Mouth Rehabilitation. International Journal of Digital Dentistry, 16(3), 113-123